On Broken Teeth: Emergency Management of Dental Fractures
Clinical Scenario: One evening in the ED, a teenage boy is brought in by his mother for dental trauma after an altercation at school. The boy reports that he was pushed to the ground in the scuffle, hitting face first into the concrete. On exam, pinkish-red material was visible at base of what remains of his frontal incisors. It's been awhile since you took care of dental trauma and you decide to read more about it.
Clinical Question: What are the different layers of teeth and how do they impact severity of dental injury? What are the risk factors for dental injury? How are dental fractures graded and what steps should the ED physician take to protect remaining tooth fragments?
Review: Traumatic dental injuries (TDI) are a common occurrence in both children and adults. Approximately 1 in 3 adults sustain dental trauma during their lifetime, the majority which occur in childhood. A wide variety of risk factors have been described in the literature. These include patient specific factors like ADHD, epilepsy, cerebral palsy, propensity for risk-taking behavior, and anatomic factors like over-jet (the horizontal distance between posterior surface of the maxillary incisors and the anterior surface of the mandibular incisors) and inadequate lip coverage. In a review of rates of TDI in epileptic patients, over half had suffered TDI, many with multiple injuries. Environmental factors include poor socioeconomic status, living in an overcrowded environment and poor road safety [1]. Etiologies of TDI are broad with the most common mechanism of injury being falls. Adolescents and adults are more likely to sustain TDI through organized sporting activities, traffic accidents and violent means including fighting and assault. In children, dental fractures can be a presentation of non-accidental trauma, and therefore a complete a full physical exam, including skin exam, should be performed.
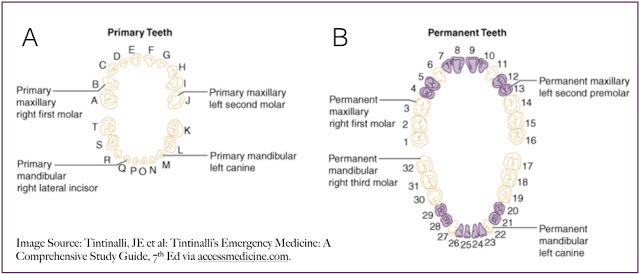
With regard to anatomy, primary dentition consists of 20 teeth – 8 incisors, 4 canines and 8 molars, classically lettered A – T. The permanent dentition includes 28 to 32 teeth – 8 incisors, 4 canines, 8 premolars and 8 - 12 molars. The 32 permanent teeth are numbered from right to left on top and left to right on the bottom [2].
With regard to anatomy of the individual teeth, from the inside out a tooth is composed of pulp, dentin and enamel [2]. The visible portion of the tooth is referred to as the crown and consists all three layers. As the tooth extends underneath the gum line, the enamel portion thins and the dentin and pulp extend in to the alveolar bone covered by a thin layer of cementum. The apex of the tooth is the entry point of the neurovascular bundle supplying each tooth. Finally, the periodontal ligament is a collagenous strructure that extends from the alveolar bone to the cementum surrounding the root of the tooth.
The primary traumatic dental injury classifications are concussion, subluxation, extrusion, luxation, intrusion, avulsion and fracture [3]. Examination of a TDI should include
visual inspection, percussion testing, manual evaluation of tooth
mobility and consideration for radiographic imaging to evaluate for
associated alveolar bone injury and widening of the periodontal ligament space.
Sensitivity testing (cold testing) is often less useful at the time of
injury due to transient lack of pulpal response.
Dental fractures aka "broken teeth" require different management based on the extent of the injury. The Ellis classification, which subdivides dental fractures into three classes of injury, is useful for ED providers because it determines emergent care of the dental fracture [4]:
- Ellis I fractures involve only the enamel. They typically require no emergency treatment. If sharp edges are present, those can be smoothed for patient comfort. Dentist follow up can be at the patient’s convenience.
- Ellis II fractures involve the dentin but not the pulp and can be identified on exam by the creamy yellow color of dentin compared to the whiter, harder enamel. These fractures require more urgent care. Because dentin is a microtubular structure, Ellis II fractures threaten the integrity of the pulp and can lead to contamination of the pulp by oral flora . After recognizing an Ellis II fracture, the ED provider should anesthetize, clean and dry the tooth (Peridex can be used to sterilize the tooth) and seal the exposed dentin, which can be done with dental cement . Urgent dental follow up in the next 24 hours is recommended. Patients will require frequent visits and radiographs.
- Ellis III fractures are full thickness and expose the pulp. They can be identified by visualization of the pink-red pulp as well as bleeding from the pulp on cleaning of the tooth. Like Ellis II injuries, the pulp is at risk with these injuries but at a greater extent given the direct exposure of pulp to the oral environment. Ellis class III injuries require a two step sealing procedure. After anesthetizing, cleaning and drying the tooth, bleeding should be controlled with careful direct pressure. The first sealant layer is a calcium hydroxide base. On top of this base, the same dental cement coverage is applied. Like Ellis II injuries, Ellis III injuries require urgent dental follow up preferably within 24 hours.
For children with injuries to primary teeth, pulp exposure is more often encountered given the relatively larger size of the pulp. The same approach to different fracture types are recommended for children. Children will often require a pulpotomy to better protect the pulp from infection, but this requires more specialized tools and can be performed by the dentist in rapid follow up.
Because dental fractures can have associated injuries, it is important to examine for associated intraoral lacerations, tooth subluxation or avulsion. Subluxations and avulsions may require repositioning of the tooth and splinting to adjacent teeth with zinc oxide based dressings like Coe-Pak [little trick of the trade: since the applications of dental splints requires teeth to be dry, cut off the end of oxygen tubing and attach to the air or oxygen on the wall to blow air onto the teeth and dry them prior to application of an adhesive dental splint].
With all of these injuries, patients should be discharged with oral analgesics, a soft diet and urgent dental follow-up. Generally, topical anesthetics should be avoided. Routine use of systemic antibiotics has not demonstrated benefit, but patient specific factors, associated injuries and co-morbidities should be considered [5].
Take-Home Points: Dental fracture management depends on the Ellis classification. Anything more than an Ellis I fracture requires some degree of a protective coating applied in the ED and referral to urgent dental follow up. Always examine patients thoroughly for other associated injuries and watch for NAT.
Submitted by Sara Manning (@EM_SaraM), PGY-4
Faculty Reviewed by Rob Poirier
Everyday EBM Editor: Maia Dorsett (@maiadorsett)
In case you were thinking that "Broken Teeth" would be a good name for a band, it's already taken. Thank you google.
References:
1. Glendor, U, “Aetiology and risk factors related to traumatic dental injuries a review of the literature.” 2009. Dental Traumatology. Vol 25: 19 – 31.
2. Tintinalli, JE et al, : Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7th Ed via Accessmedicine.com
3. Dentaltraumaguide.org
4.DiAngelis et al, “International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth.” 2012 Dental Traumatology. Vol 28: 2 – 12.
5. ANDREASEN, J. O., STORGÅRD JENSEN, S. I. M. O. N., & SAE‐LIM, V. A. R. A. W. A. N. (2006). The role of antibiotics in preventing healing complications after traumatic dental injuries: a literature review. Endodontic Topics, 14(1), 80-92.
Theme Image Source: http://www.windsorstar.com
Clinical Question: What are the different layers of teeth and how do they impact severity of dental injury? What are the risk factors for dental injury? How are dental fractures graded and what steps should the ED physician take to protect remaining tooth fragments?
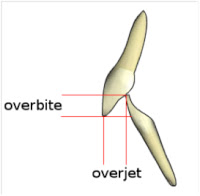 |
| Source: wikipedia.org |
With regard to anatomy, primary dentition consists of 20 teeth – 8 incisors, 4 canines and 8 molars, classically lettered A – T. The permanent dentition includes 28 to 32 teeth – 8 incisors, 4 canines, 8 premolars and 8 - 12 molars. The 32 permanent teeth are numbered from right to left on top and left to right on the bottom [2].
With regard to anatomy of the individual teeth, from the inside out a tooth is composed of pulp, dentin and enamel [2]. The visible portion of the tooth is referred to as the crown and consists all three layers. As the tooth extends underneath the gum line, the enamel portion thins and the dentin and pulp extend in to the alveolar bone covered by a thin layer of cementum. The apex of the tooth is the entry point of the neurovascular bundle supplying each tooth. Finally, the periodontal ligament is a collagenous strructure that extends from the alveolar bone to the cementum surrounding the root of the tooth.
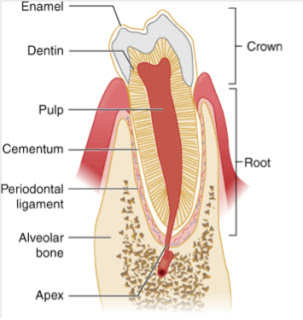 |
Image source: Tintinalli, JE et al: Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7th
Ed via Accessmedicine.com
Dental fractures aka "broken teeth" require different management based on the extent of the injury. The Ellis classification, which subdivides dental fractures into three classes of injury, is useful for ED providers because it determines emergent care of the dental fracture [4]:
- Ellis I fractures involve only the enamel. They typically require no emergency treatment. If sharp edges are present, those can be smoothed for patient comfort. Dentist follow up can be at the patient’s convenience.
- Ellis II fractures involve the dentin but not the pulp and can be identified on exam by the creamy yellow color of dentin compared to the whiter, harder enamel. These fractures require more urgent care. Because dentin is a microtubular structure, Ellis II fractures threaten the integrity of the pulp and can lead to contamination of the pulp by oral flora . After recognizing an Ellis II fracture, the ED provider should anesthetize, clean and dry the tooth (Peridex can be used to sterilize the tooth) and seal the exposed dentin, which can be done with dental cement . Urgent dental follow up in the next 24 hours is recommended. Patients will require frequent visits and radiographs.
- Ellis III fractures are full thickness and expose the pulp. They can be identified by visualization of the pink-red pulp as well as bleeding from the pulp on cleaning of the tooth. Like Ellis II injuries, the pulp is at risk with these injuries but at a greater extent given the direct exposure of pulp to the oral environment. Ellis class III injuries require a two step sealing procedure. After anesthetizing, cleaning and drying the tooth, bleeding should be controlled with careful direct pressure. The first sealant layer is a calcium hydroxide base. On top of this base, the same dental cement coverage is applied. Like Ellis II injuries, Ellis III injuries require urgent dental follow up preferably within 24 hours.
For children with injuries to primary teeth, pulp exposure is more often encountered given the relatively larger size of the pulp. The same approach to different fracture types are recommended for children. Children will often require a pulpotomy to better protect the pulp from infection, but this requires more specialized tools and can be performed by the dentist in rapid follow up.
Because dental fractures can have associated injuries, it is important to examine for associated intraoral lacerations, tooth subluxation or avulsion. Subluxations and avulsions may require repositioning of the tooth and splinting to adjacent teeth with zinc oxide based dressings like Coe-Pak [little trick of the trade: since the applications of dental splints requires teeth to be dry, cut off the end of oxygen tubing and attach to the air or oxygen on the wall to blow air onto the teeth and dry them prior to application of an adhesive dental splint].
With all of these injuries, patients should be discharged with oral analgesics, a soft diet and urgent dental follow-up. Generally, topical anesthetics should be avoided. Routine use of systemic antibiotics has not demonstrated benefit, but patient specific factors, associated injuries and co-morbidities should be considered [5].
Take-Home Points: Dental fracture management depends on the Ellis classification. Anything more than an Ellis I fracture requires some degree of a protective coating applied in the ED and referral to urgent dental follow up. Always examine patients thoroughly for other associated injuries and watch for NAT.
Submitted by Sara Manning (@EM_SaraM), PGY-4
Faculty Reviewed by Rob Poirier
Everyday EBM Editor: Maia Dorsett (@maiadorsett)
In case you were thinking that "Broken Teeth" would be a good name for a band, it's already taken. Thank you google.
References:
1. Glendor, U, “Aetiology and risk factors related to traumatic dental injuries a review of the literature.” 2009. Dental Traumatology. Vol 25: 19 – 31.
2. Tintinalli, JE et al, : Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7th Ed via Accessmedicine.com
3. Dentaltraumaguide.org
4.DiAngelis et al, “International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth.” 2012 Dental Traumatology. Vol 28: 2 – 12.
5. ANDREASEN, J. O., STORGÅRD JENSEN, S. I. M. O. N., & SAE‐LIM, V. A. R. A. W. A. N. (2006). The role of antibiotics in preventing healing complications after traumatic dental injuries: a literature review. Endodontic Topics, 14(1), 80-92.
Theme Image Source: http://www.windsorstar.com