A 69 y.o. male comes to the ED with sudden hearing loss in the R ear. It worsened over several hours and now he cannot hear out of the R ear.
What should be in your differential?
Hint: the eardrum is normal.
A review of the anatomy of the tympanic membrane
Our patient had sudden sensorineural hearing loss.( SSNHL). . This is a rapid loss of hearing that occurs over 72 hrs. It is a medical emergency because early steroids offer the best chance for the recovery of hearing. Although about half of the people with SSHL will recover in one to two weeks; in some the hearing loss is permanent.
It often affects people in their 40’s and 50’s . most cases are idiopathic but viral and autoimmune causes have been documented. Many other causes have been postulated for the syndrome including Lyme disease, syphilis, drugs and neoplasms.
Multiple cases were attributed to COVID. Research has shown that SARS--CoV-2 can access the inner ear through the olfactory nerve. In addition to loss of taste and smell, it can it is thought that it could access the vestibular nerve in the same way causing deafness.
Hearing loss is the most common sensory deficit globally with one in five people affected. In the US it affects 23% of individuals 12 or older. Exposure to loud noise is still the most common reason for hearing loss.
BEWARE-the MRI image below is from a 62 y.o. with acute unilateral hearing loss who had a stroke.
T2 weighted images showing hyperintense foci in the L middle cerebral peduncle. The problem is this was six days after the hearing loss and emphasizes the fact that posterior strokes can be missed on MRI.
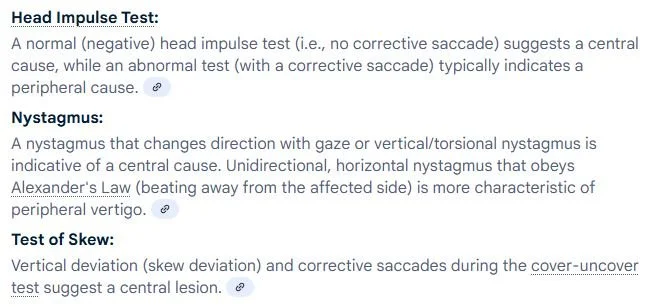
A stroke pr TIA can present as isolated acute hearing loss. This was documented in the development of the HINTS exam. The strokes that were missed were posterior circulation strokes in the posterior inferior cerebellar artery (PICA) or anterior inferior cerebellar artery (AICA) territory. It is known that AICA territory strokes are more likely to mimic a peripheral vestibulopathy closely; this is because the AICA generally supplies blood to the inner ear (including labyrinth), vestibular nerve root entry zone, and flocculus each of which, when infarcted, can lead to a unilaterally abnormal HINTS test. This raises another bit of confusion since the HINTS test should be normal (negative/no corrective saccade) in a central lesion. This is the same result if the HINTS is done on a normal person without signs of acute vestibular syndrome (AVS).
Some patients with AVS have neither gaze-evoked nystagmus nor skew deviation, creating a peripheral pattern HINTS result, despite the presence of a stroke. Adding a fourth clinical sign (unilateral acute hearing loss) to HINTS (ie, HINTS+) “rescues” some of these sensitivity losses . It is recommended that hearing and orthostatic vitals always be checked in these patients.
IN SUMMARY
Give steroids immediately when acute hearing loss presents because it is shown to improve recovery.
A stroke can present as acute hearing loss in isolation. Consider risk factors prior to diagnosis in acutely “dizzy” patients and test their hearing.
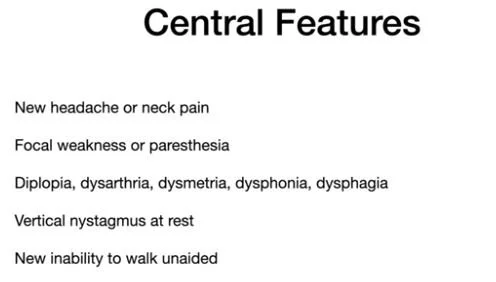
Our patient started on steroids and completely recovered his hearing in four days. If you have forgotten the HINTS exam, a review follows. Do not do a HINTS exam if central features are present.
do not do a HINTS unless nystagmus is present
skew is the most sensitive and hardest to detect Nystamus should be done at rest and looking to the sides through a sheet of paper to prevent fixation which decreases nystagmus.
Zhong Y, Hongyan L, Liu G Early detection of stroke at the sudden sensorineural hearing loss stage. Front Neurol. 2023 Nov 1;14:1293102.
Tarnutzer A, Gold D, Wang Z. Impact of clinician training background and stroke location on bedside diagnostic accuracy in the acute vestibular syndrome- a meta-analysis. Ann Neurol 2023 Apr 27;94(2):295-308.
Bai X, Chen S, Xu K, Jin Y, Niu X, Xie L, et al. N-acetylcysteine combined with dexamethasone treatment improves sudden sensorineural hearing loss and attenuates hair cell death caused by ros stress. Front Cell Dev Biol. (2021) 9:659486. 10.3389/fcell.2021.659486 N-acetylcysteine plus intratympanic dex.
Najafloo R, Majidi J, Asphari A, et al. Mechanism of anosmia caused by symptoms of COVID-19 and emerging treatments. ACS Chemical Neuroscience Vol 12(20)
Koumpa F, Forde C, Manjaly J. Sudden irreversible hearing loss post COVID-19. BMJ Case Reports CP 2020;13e238419.
Hirt Z, Kohanzadeh A, Gibber M. Sensorineural hearing loss as a complication of COVID-19 and the COVID-19 vaccine. Cureus doi:10.7759/cureus.47582.
Lee H, Sohn S, Jung D. Sudden deafness and anterior inferior cerebellar artery infarction. Stroke 2002. Vol 33(12).
Kuhn M, Heman=Ackah S, Shaikh J, et al Sudden Sensorineural hearing loss: A review of diagnosis, treatment and prognosis. 2011 Sept;15(3):91-105
https://www.youtube.com/watch?v=1q-VTKPweuk Peter Johns