A 78 y.o. woman presents with weakness and a bluish discoloration of her nose
What is your differential?
our patient has lymphoma
Our patient had catastrophic antiphospholipid syndrome(cAPS) associated with lymphoma. This caused diffuse clotting in the small vessels leading to dermal ischemia. Antiphospholipid syndrome (APS) occurs in many hematologic neoplasms including Hodgkin’s lymphoma and non hodgkin’s lymphoma. It is estimated that 35% of newly diagnosed lymphoma patients have APS. The syndrome is different from just having antiphospholid antibodies (aPL) which can be present without causing thrombosis.
The complicated chart of how APS is diagnosed.
Trousseau in 1895 first described the thrombotic occlusions in patient with carcinoma, but antiphospholipid syndrome was first described in lupus. much later. Antiphospholipid antibodies bind to endothelial cell surfaces activating platelets and leukocytes leading to thrombosis. The major types of antiphospholipid antibodies are lupus anticoagulant, anticardiolipin, anti beta 2 glycoprotein and antiprothrombin. Cryoglobulins are NOT antiphopholipid antibodies but could account for a bluish discoloration of the nose as seen in our patient.
A patient with cryoglobulins, no vasculitis on biopsy and an ischemia nassal tip which responded to steroids.
While cancers (both solid tumors and hematologic malignancies) can cause secondary APS and autoimmune diseases like lupus cause primary APS, there are many other conditions in which antiphospholipid antibodies (aPL) are found. Syphilis was the first infection in which antiphospholipid antibodies were found. A false positive RPR(Rapid Plasma Reagin) can occur in patients with lupus who have aPL.
Covid-19 showed microvascular events in a small number of patients and these were associated with high titers of antiphopholipid antibodies. 40% of covid patients are positive for lupus anticoagulant in some studies. To muddy the waters, The covid vaccine itself has been implicated in APS.
livido retiularis and covid toes are associated with aPL in covid
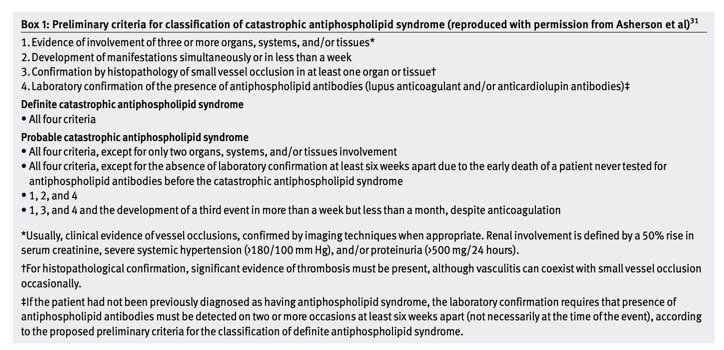
While it seems that antiphospholipid antibodies are common in many situations, there is a catastrophic antiphospholipd syndrome (cAPS) which develops rapidly after a trigger. The trigger can be obstetric, traumatic or infectious and often occurs in patients with a primary antiphospholipid syndrome. If this occurs, mortality is very high with SIRS and ARDS followed by organ failure. Current treatment for this condition is plasma exchange. In patients with underlying lupus, hydroxychloroquine is protective against thrombosis.
The clues that APS may be present include: prolonged PTT, + Coombs, a pregnancy loss or complication and a hx of DVT.
Vitamin K antagonists and supportive care remain the treatment for APS.
Our patient had widely metastastic lymphoma, was negative for cryoglobulins and had aPL antibodies. She was admitted to the hospital and expired.
Nagua M, Joshi A. COVID-19 vaccine: culprit or innocent bystander in a rare adverse gastrointestinal surgical event: a case report with review of the literature. J. Fdamily Med PrimCare. 2024 Mday;13(5):2152-2156.
Lindquist M, VigiBase . The SHO global ICSR database system. Basic facts. Ther Innov Regul Sci. 2008;42:409-18,
Chora C, Guimaraes S, Julio S, Vaz-Marques P. Nasal skin necrosis: a very rare manifestation of antiphospholipid syndrome. EJCRIM2016:3 doi 10.12890/2016_000534fg
Butt A, Erkan D, Lee A. Covid-19 and antiphospholipid antibodies. Best Pract Res CLin Haematol 2022 Sep;35(3):101492.
Asherson R. Cervera R. Antiphospholipid antibodies and infection. Ann Rheum Dis 2003;62:388-393