A 22 y.o. comes in with a rash; it began 3 weeks ago as papules and now has become necrotic.
what could cause this?
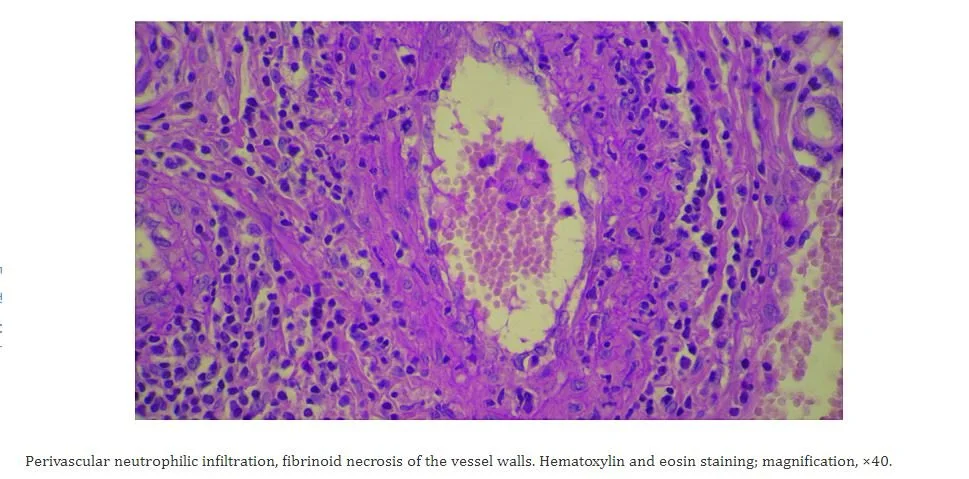
Our patient had leukocytoclastic vasculitis. This is a small vessel vasculitis mediated by immune complexes in the dermal capillaries and venules. These complexes recruit neutrophils by attaching to the Fcy receptors on neutrophils. The neutrophils then attach to vessel walls and cause necrosis (caused by lysosomal enzymes and free radicals) allowing the neutrophils to move into the surrounding tissue.
biopsy is diagnostic for leukocytoclastic vasculitis.
The increased venous pressure in the legs is why it tends to occur first in the lower extremities. The findings of leukocytoclastic vasculitis are often confined to the skin but in 30% of cases other organs can be involved. In Henoch Schonlein purpura, which is IgA mediated, the intestine or kidneys can be involved. In 90% of cases the rash disappears in weeks.
Henoch Scholein purpura is IgA related thought to be post viral, occurs in children ages 2-5 and may affect the bowel or kidneys.
Immune complex-mediated small vessel vasculitis can be seen in rheumatoid arthritis, lupus, Sjogren’s Henoch-Schonlein purpura, cryoglobulinemia, inflammatory bowel disease, and urticarial vasculitis. In addition to these conditions: drugs, infections (hep B, hep C and syphilis) and paraneoplastic syndromes can cause this vasculitis.
Leukocytoclastic vasculitis is idiopathic in about 50% of cases. If autoimmune diseases are ruled out Infections and drugs are the next most common triggers.
This is a review of necrotic skin lesions caused by immune-complex deposition. However, lack of blood flow and injuries,often related to neuropathy, can also cause necrosis.
In frostbite, cold causes vasoconstriction and tissue ischemia. “Winter is coming” (the Starks)
The treatment for leukocytoclastic vasculitis is steroids. Our patient was admitted for solumedrol and then switched to prednisone. In our patient rheumatologic, infectious and drug related causes were ruled out. He is one of the 50% of patients where no cause is ever found. He improved on steroids and is still on a tapering dose.
FeketeK, FeketaL. Cutaneous leukocytoclastic vasculitis associated with erlotinib treatment: A case report and review of the literature. Exp Ther Med 2019 Feb;17(2):1128-1131.
Williams M, Azcutia V, Newton G, et al. Emerging mechanisms of neutrophil recruitment across endothelium. Trends Immunol 2011 Oct;32(10):461-469.
Motta I, Perricone G. Ulcerative pyodema gangrenosum in inflammatory bowel disease Clinical Picture vol.(4) issue 6, p 488 June 2019.