A 35 y.o. male truck driver had a seizure in his vehicle. He co L shoulder pain.
What do you notice on his xray? What needs to be done next?
Hint: he has a posterior dislocation of the shoulder and his Na is 117.
Our patient had a posterior shoulder dislocation after a seizure. These can be difficult to see on xray with an estimated 50% being missed. An axillary view is needed to make the diagnosis
More importantly, the patient’s sodium was 117 because he had COVID pneumonia which was visible on the shoulder xray. So the question became whether he became hyponatremic from dehydration or SIADH. He was given normal saline initially and seized for a second time.
He fit the criteria for SIADH with serum osmolatlity <275 mOsm/kg, urine osmolality > 100 and urine Na > 40 He was given 3% Na and admitted to the ICU.
In the ICU his Na initially dropped to 119 and then rose to 142 in one day. The goal is actually 6 amEq rise in 24 hours. The rapid rise puts him at risk for central pontine myelinolysis. Rapid rise in sodium was corrected by giving D5 and a DDAVP clamp/bolus treatment.
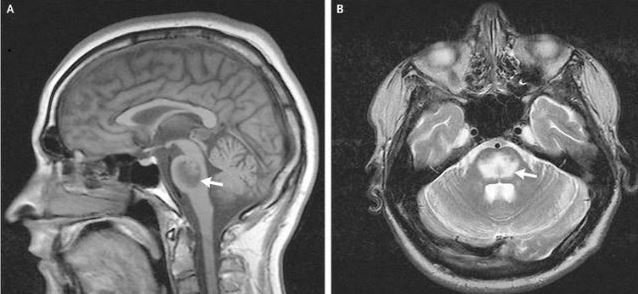
central pontine myelinolysis from alcoholism
HYPONATREMIA MANAGEMENT
SIADH is a condition where water handling is out of balance because there is too much ADH( antidiuretic hormone). This can be caused by pituitary surgery, lung disease, drugs or infection. If you administer 1 L of NS to a patient with SIADH all of the sodium will be excreted and half of the water so the patient actually becomes more hyponatremic. The recommendation is to restrict fluid and give 3 % NS. But how do you avoid correcting the Na too quickly? DDAVP in small boluses can help avoid the problem because DDAVP increases urine concentration and avoids free water loss This is what is referred to an the DDAVP clamp.
MDCalc is an app which can calculate the change in sodium over time and tells you how much 3% saline to give. For a 70 kg male with a sodium of 117 it recommends 0.5mEq/L/hr. This is 53 ml/hr of 3% saline.
By giving the patient free water and correcting the sodium more gradually his sodium was corrected. He did not have central pontine myelinolysis and was discharged with outpatient ortho follow up.
Moroder P, Danzinger V, Minkus M, et al. the ABC guide for the treatment of posterior shoulder instability Orthopade. 2018 Feb;47(2):139-147.
Fleming J, Babu S. Central Pontine Myelinolysis NEJM 2008; Dec 4. 359:e29.
Decaux G, Musch W. Clinical laboratory evaluation of the syndrome of inappropriate secretion of antidiuretic hormone. Clin J Am Soc Nephrol 2008;3(4):1175-1184.