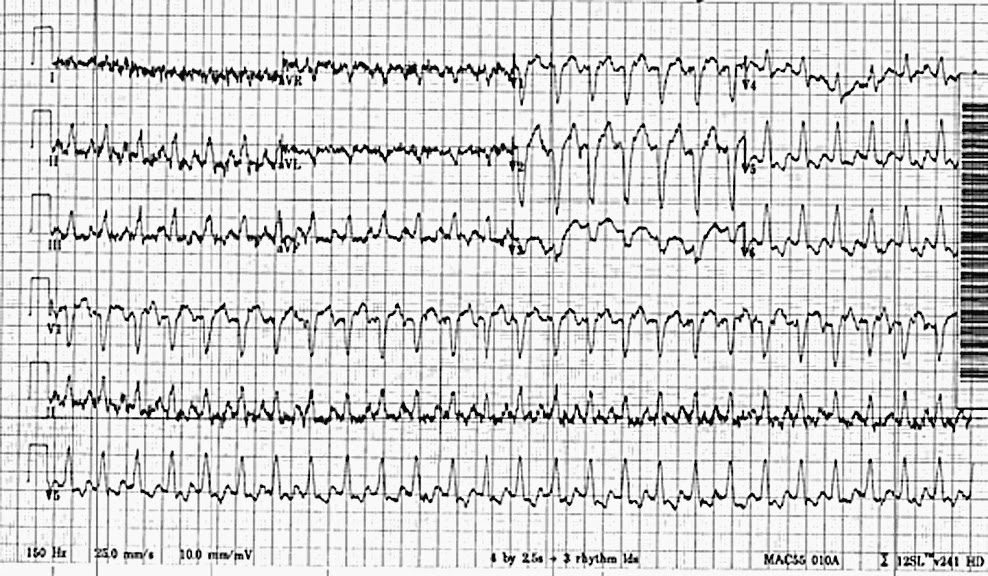
EKG Challenge No. 11 - Mmmm.... That looks sort of fast...
You are
working one evening in the emergency department when a 60-something year
old female is slotted for a room. Her chief complaint? "Fever,
weakness, vomiting". Seeing that her triage heart rate was 157, you
leave your granola bar where it is and immediately walk into the room to
assess her. You see an elderly-appearing female in moderate
respiratory distress. Her temperature is 38.2, blood pressure is
125/87, RR is 32, oxygen saturation is 93% on 5L NC. She has a history
of a bone-marrow transplant and is chronically immunosuppressed. She
endorses poor PO intake and several episodes of emesis over the last few
days. She says that she came in today when she developed some
shortness
of breath as well. She denies any chest pain or palpitations. On exam,
her mucous
membranes are dry, her abdomen non-tender, and her breath sounds are
decreased in the right base. You are a bit disturbed by the looks
of her rhythm strip on the monitor so
you get a 12-lead EKG:
Interpret the EKG. What is your differential? What would you do next?
See the case conclusion here.