EKG Challenge No. 11 Case Conclusion: It's Wide! It's Fast! It's a Wide Complex Tachycardia!
You are
working one evening in the emergency department when a 60-something year
old female is slotted for a room. Her chief complaint? "Fever,
weakness, vomiting". Seeing that her triage heart rate was 157, you
leave your granola bar where it is and immediately walk into the room to
assess her. You see an elderly-appearing female in moderate
respiratory distress. Her temperature is 38.2, blood pressure is 125/87, RR is 32, oxygen saturation is 93% on 5L NC. She has a history of a bone-marrow transplant and is chronically immunosuppressed. She
endorses poor PO intake and several episodes of emesis over the last few
days. She says that she came in today when she developed some shortness
of breath as well. She denies any chest pain or palpitations. On exam, her mucous
membranes are dry, her abdomen non-tender, and her breath sounds are decreased in the right base. You are a bit disturbed by the looks
of her rhythm strip on the monitor so
you get a 12-lead EKG:
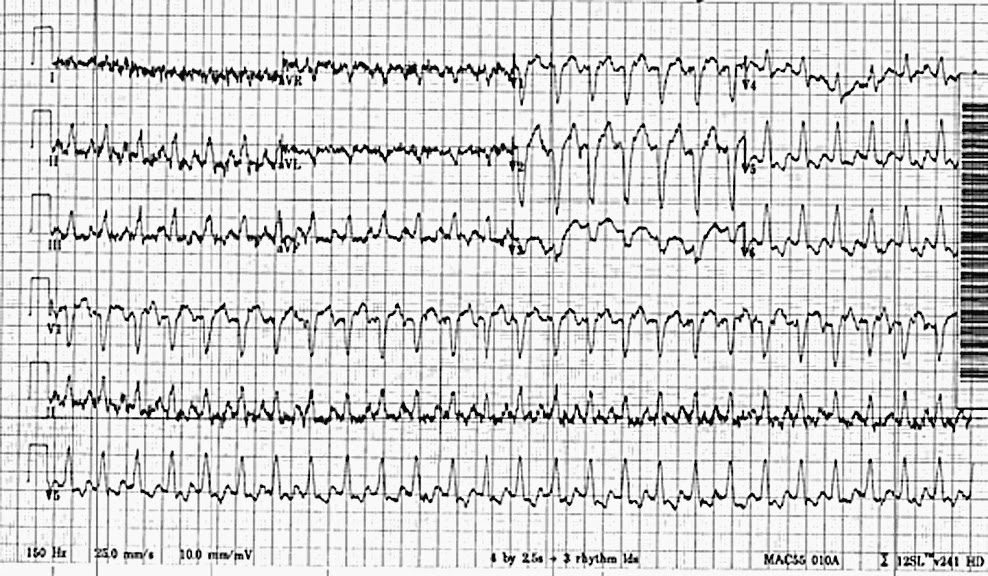
The EKG above features a regular tachycardia (rate of 162) with a QRS complex duration of > 120 ms with LBBB morphology. This leads you to an initial EKG diagnosis of a regular wide complex tachycardia, which has the following differential [1,2,3]:
Originates in the ventricle:
1. Ventricular tachycardia
Originates above the ventricle, but has abnormal ventricular conduction:
2. Supraventricular tachycardia (AVRNT) with delayed ventricular conduction
3. Atrial flutter with 2:1 block and delayed ventricular conduction
4. Sinus tachycardia with delayed ventricular conduction
Delayed ventricular conduction can be due to a pre-existing bundle branch block, a toxicologic insult leading to QRS widening (such as Na-channel blockade), electrolyte abnormality (such as hyperkalemia), or aberrancy. Aberrancy refers to the situation in which one bundle branch is ready to conduct another beat, but the other has not had time to fully repolarize and occurs in the setting of tachycardias in which there is a very short interval between electrical impulses.
So how and why does one differentiate between these three scenarios? Since we are emergency providers in the business of saving lives, the important consideration at each step of working through an EKG differential is considering how making the "EKG diagnosis" will alter patient management.
Since the management of sinus tachycardia is to treat the underlying cause (and not electricity or anti-arrythmmics), the first step of working through the differential is differentiate Sinus tachycardia with abnormal conduction from SVT with aberrancy and Vtach by asking
Are there sinus p-waves?
We underline the term sinus here because with SVT and Vtach you can get retrograde or abnormal p-waves. To remind everyone, p-waves need to meet the following criteria for the rhythm to be considered sinus:
- a p-wave in front of every QRS
- Normal p wave axis: upright in I, II; inverted in aVR; biphasic in V1.
If you can find a prior EKG for the patient with the same bundle branch block morphology, this lends further evidence to your cause.
If it is sinus tachycardia, then identify and treat the underlying cause. If it is not sinus tachycardia, then you are left with two possibilities: SVT with aberrancy or Vtach.
Many algorithms have been developed to differentiate between these two conditions [5,6,7]. For those of you who are interested, more detailed descriptions of these algorithms are included at the very end of this post.
The truth of the matter is that when there are more than five algorithms (and there are!) to differentiate between two conditions, it is likely that none of them are good enough to use in a life and death situation such as this one. Indeed, one recent study by Szelenyi et. al. compared the "real life" sensitivity of two different recently developed algorithms (RWPT in II and Vereckei's avR algorithm) when applied by cardiologists, internists and emergency physicians [8]. Both algorithms were insufficiently sensitive for Ventricular tachycardia in this real life application:
Similarly, another study published by Kastrzebski et. al. found that the performance of multiple algorithms, including those cited above, was sub-par for real life use:
 |
| Image source: Reference 8 |
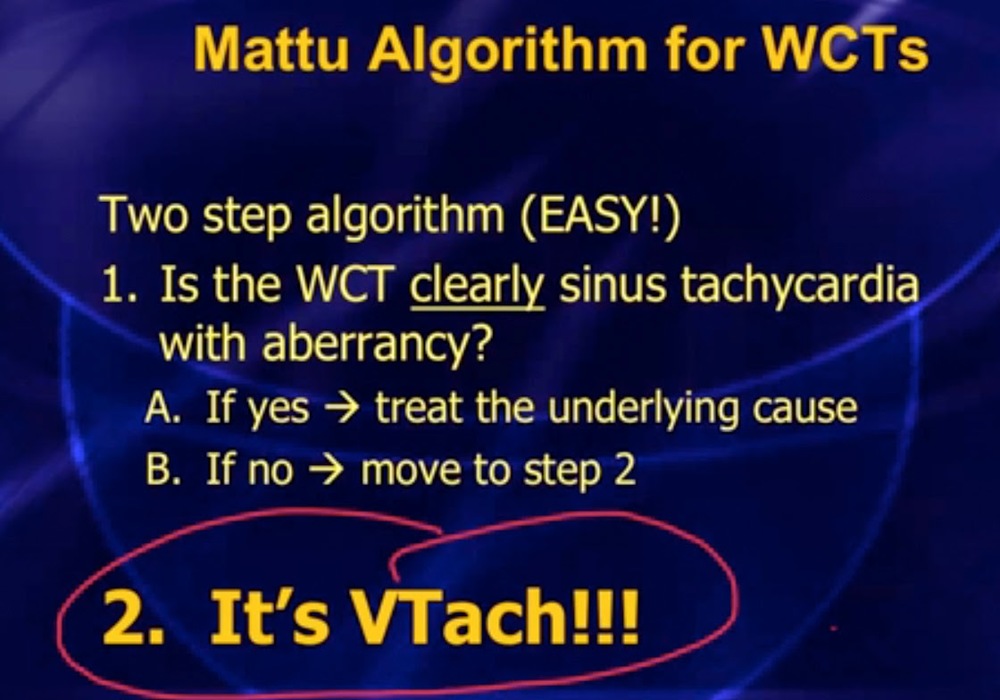
Therefore, if you are an "EP" as in Emergency Provider rather than Electrophysiologist, you should probably subscribe to the Mattu algorithm for management of wide complex tachycardias which he presented in this episode of the ECG case of the week:
Getting back to our case, you apply the Mattu algorithm to your patient.
Step 1: Is the rhythm sinus?
You examine the EKG and find upright p-waves in lead II:
After 1 liter of fluid her heart rate comes down and you can see this even more clearly:
Your EKG diagnosis? sinus tachycardia with LBBB.
Your emergency department management? Treat the underlying cause.
Given that this is an immunosuppressed patient with fever and tachycardia, you have high suspicion for sepsis. Blood and urine cultures sent. A CXR reveals an underlying right-sided pneumonia.
The patient is started on broad spectrum antibiotics and ultimately does well. Score: EP 1, Sepsis 0.
Take home Points: Wide complex tachycardias have an important differential diagnosis. Start by determining if the rhythm is sinus, because this requires treating the underlying cause such as sepsis, PE, dehydration or pain. If the rhythm is not sinus, assume its ventricular tachycardia because even if you had the time, no algorithm is sensitive or specific enough to rule out Vtach. Electricity helps both and should be used in the unstable patient. Remember, it's safer in the long run to assume it's T-rex and not a Tweety bird:
Submitted by Maia Dorsett (@maiadorsett), PGY-3
Faculty reviewed by Douglas Char
References:
[1]Goldberger, Z. D., Rho,
R. W., & Page, R. L. (2008). Approach to the diagnosis and initial
management of the stable adult patient with a wide complex tachycardia. The American journal of cardiology, 101(10), 1456-1466.
[2]Brady, W. J., & Skiles, J. (1999). Wide QRS complex tachycardia: ECG differential diagnosis. The American journal of emergency medicine, 17(4), 376-381.
[3]Hollowell, H., Mattu, A.,
Perron, A. D., Holstege, C., & Brady, W. J. (2005). Wide-complex
tachycardia: beyond the traditional differential diagnosis of
ventricular tachycardia vs supraventricular tachycardia with aberrant
conduction. The American journal of emergency medicine, 23(7), 876-889.
[4]Brugada, P., Brugada, J.,
Mont, L., Smeets, J. L. R. M., & Andries, E. W. (1991). A new
approach to the differential diagnosis of a regular tachycardia with a
wide QRS complex. Circulation, 83(5), 1649-1659.
[5] Pava, L. F., Perafán, P.,
Badiel, M., Arango, J. J., Mont, L., Morillo, C. A., & Brugada, J.
(2010). R-wave peak time at DII: a new criterion for differentiating
between wide complex QRS tachycardias. Heart Rhythm, 7(7), 922-926.
[6]Vereckei, A., Duray, G.,
Szénási, G., Altemose, G. T., & Miller, J. M. (2008). New algorithm
using only lead aVR for differential diagnosis of wide QRS complex
tachycardia. Heart Rhythm, 5(1), 89-98.
[7]Szelényi, Zsuzsanna, et
al. "Comparison of the “Real‐life” Diagnostic Value of Two Recently
Published Electrocardiogram Methods for the Differential Diagnosis of
Wide QRS Complex Tachycardias." Academic Emergency Medicine 20.11 (2013): 1121-1130.
[8] Jastrzebski, M., Kukla,
P., Czarnecka, D., & Kawecka-Jaszcz, K. (2012). Comparison of five
electrocardiographic methods for differentiation of wide QRS-complex
tachycardias. Europace, 14(8), 1165-1171.
Still up for a little more learning? Here is a summary of three of the algorithms for distinguishing SVT with aberrancy vs. Vtach. Below is a summary of three of them as well as links to additional resources.
i. The Brugada algorithm:
One of the most well-known criteria for differentiating SVT with
aberrancy vs Vtach. It comprises a series of four questions. If the
answer to any question is "Yes" then the diagnosis is Ventricular
tachycardia [5].
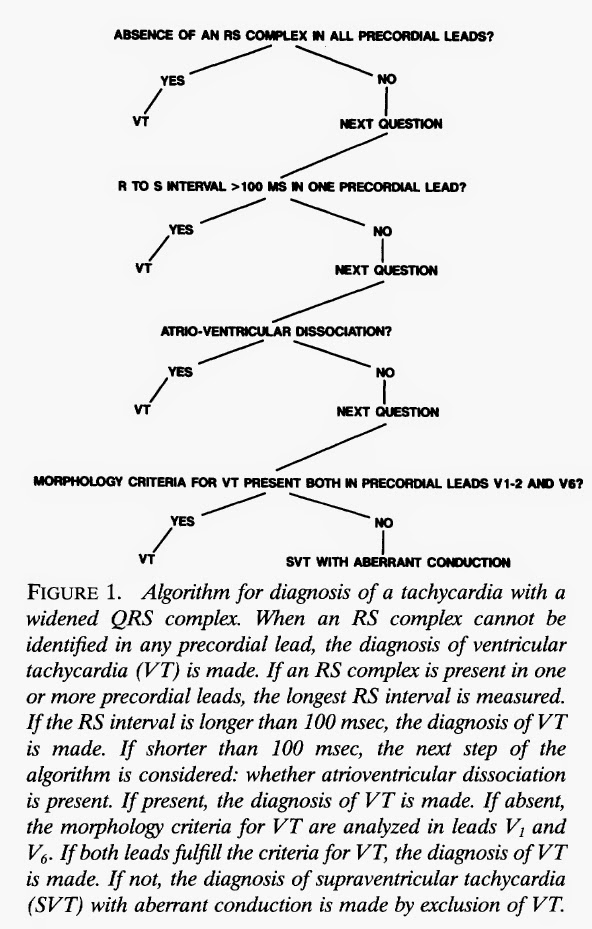 |
| Brugada algorithm; Figure 1 from Reference 5. |
You can link to the PV Card from ALiEM for the Brugada criteria here.
ii. R-wave to peak time at DII:
This algorithm (also from Brugada) was published in 2010 as an attempt
to develop simpler criteria utilizing only one lead [6]. It was
developed using an EP study as a gold standard. The basic premise is
that if the R wave to peak time (duration from the onset of QRS
depolarization onset until the first change of polarity) is >
50 ms in lead II, the diagnosis is Vtach. The authors reported a
sensitivity and specificity for Vtach of 0.93 and 0.99, respectively.
 |
| RWPT in lead II measurement. Figures 5 & 6 from Reference 6. |
One
thing that you can see from their example (above) is that measuring
RWPT really is not that straightforward. And practically speaking, a
sensitivity of 93% really is not good enough. You can read more about
this method at ALiEM here.
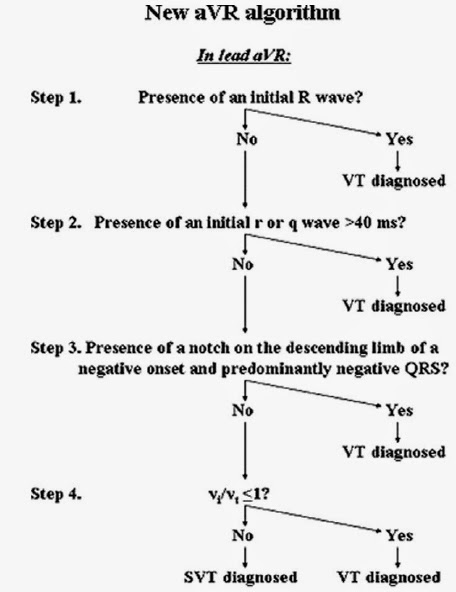
iii. Vereckei's algorithm for lead aVR, published in 2008, uses lead aVR to differentiate from Vtach vs. SVT with aberrancy:
The
last step of this algorithm, Step 4, requires a calculated comparison
of the distance traveled during the initial and concluding impulses of
the QRS complex:
In the initial study, they reported a 96.5% sensitivity for the diagnosis of Ventricular tachycardia.