Gettin' jiggy wit it ... Stick a Catheter in it? Consider the Peripheral IJ.
 Clinical scenario: You are taking care of a patient with a history of IV drug use who presents to the emergency department with a large abscess in her arm requiring drainage under conscious sedation. Nursing is unable to obtain IV access after multiple attempts. You look for an EJ or an ultrasound-guided peripheral IV and find no suitable sites. The patient is likely to be discharged so a central line seems unnecessary. You scope out the patient's neck under ultrasound and see the plump internal jugular (IJ) vein and wonder, why don't I just put an IV in that?
Clinical scenario: You are taking care of a patient with a history of IV drug use who presents to the emergency department with a large abscess in her arm requiring drainage under conscious sedation. Nursing is unable to obtain IV access after multiple attempts. You look for an EJ or an ultrasound-guided peripheral IV and find no suitable sites. The patient is likely to be discharged so a central line seems unnecessary. You scope out the patient's neck under ultrasound and see the plump internal jugular (IJ) vein and wonder, why don't I just put an IV in that? Clinical Question: Is there any literature to support or refute the use of the peripheral IV in a central vein?
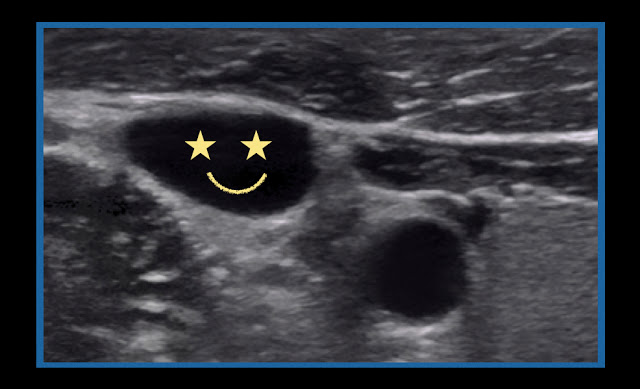
Literature Review: In patients who are critically ill with difficult IV access, the decision to move forward with intraosseous or central venous access is relatively clear. However, stable patients requiring intravenous access that have no sites amenable to ultrasound guided peripheral IVs or external jugular access and are likely to be discharged present more of a conundrum.
One proposed alternative to placement of central venous access for these patients is the "peripheral IJ", an angiocatheter placed into the internal jugular vein. Anatomically speaking, a "peripheral IJ" is not a central line. Like the external jugular vein, which also drains into the subclavian, the catheter tip is far superior to the cavo-atrial junction and thus does not constitute central access.
In 2009, a Letter to the Editor published in the Journal of Emergency Medicine described a technique in which the internal jugular was cannulated under ultrasound guidance with a 48 mm -peripheral angio catheter. The technique described involved the following steps:
1. Place the patient in trendelenberg
2. Prep the neck with chlorhexadine as you would for a central line
3. Use a linear ultrasound probe covered in a sterile probe cover and sterile gel to identify the internal jugular vein
4. Cannulate the vein and advance catheter over needle
5. Flush & Dress with bio-occlusive dressing
No sterile drapes were used.
In the report, the technique (anecdotally) had been safely performed many times, but presented no supporting data.
Following this initial letter, two subsequent case series have been published supporting the peripheral-IJ as a reasonable alternative for temporary venous access. The first case series of 9 patients placed them in patients with unobtainable IV access [2]. 64 mm angiocatheters were used to cannulate the IJ under ultrasound guidance using the above-described technique. All catheters were labeled for removal within 72 hrs. All patients were followed up via chart review one year later. Two of 9 catheters failed due to kinking within the first 48 hrs. There were no apparent adverse outcomes in any patient including deep vein thrombosis, bacteremia, endocarditis or pneumothorax. A second group conducted a prospective case series in which 9 patients underwent placement of a ‘‘peripheral IJ” (PIJ), when other access could not be obtained and the patient did not initially require a central line [3]. The authors attempted follow-up with all patients within a week. On follow-up, the seven patients who were successfully contacted denied any fevers, chills, swelling or pain at the site of catheter entry. One likely reason for the decrease in complication rate is that the placement of a "peripheral IJ" does not require dilation of the vessel.
Take Home: In the patient with a need for short-term intravenous access and in whom ultrasound peripheral IVs or external jugular access cannot be obtained, consider placement of a peripheral-IJ. This procedure should be completed under sterile precautions above that used for standard ultrasound guided IV. Larger studies are needed to verify the safety of this technique on a broader scale. If you’re patient is morbidly obese (a common theme for difficult IV access) keep in mind that an even longer IV catheter may be required to keep it safely intravenous after placement.
Submitted by Daniel Kolinsky, PGY-3
Edited by Maia Dorsett (@maiadorsett), PGY-4
Faculty Reviewed by Evan Schwarz
References
1. Moayedi S. Ultrasound-guided venous access with a single lumen catheter into the internal jugular vein. J Emerg Med 2009;37:419.
2. Zwank, M. D. (2012). Ultrasound-guided catheter-over-needle internal jugular vein catheterization. The American journal of emergency medicine, 30(2), 372-373.
3. Teismann, N. A., Knight, R. S., Rehrer, M., Shah, S., Nagdev, A., & Stone, M. (2013). The ultrasound-guided “peripheral IJ”: internal jugular vein catheterization using a standard intravenous catheter. The Journal of emergency medicine, 44(1), 150-154.