A 65 y.o. woman presented with hypoxia and hypotension secondary to influenza. She was intubated and a L IJ was placed.
you are being asked to confirm line placement
Where is it?
Our patient had a venous line in a L sided SVC. A CT of the venous anatomy in the chest is shown below. The L sided SVC drains into the coronary sinus and R atrium. The L sided SVC is the most common thoracic venous anomaly and may be associated with cardiac abnormalities.
this is a line in the L svc draining to the coronary sinus
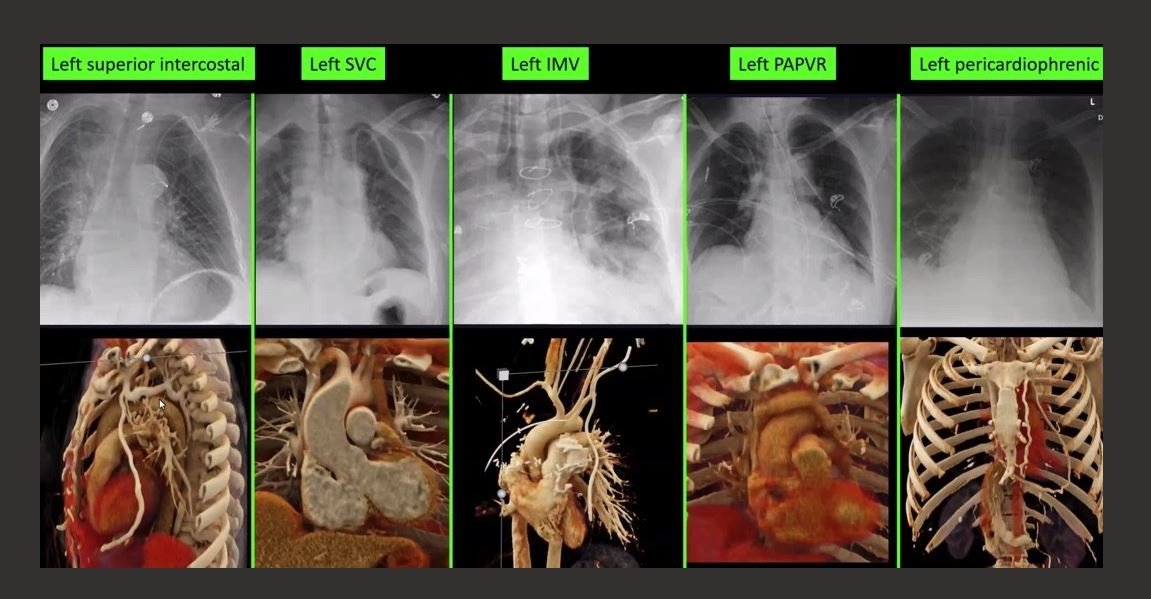
Congenital anomalies and even an abnormal course in a patient with normal anatomy can make interpreting the central line placement difficult. A few unusual paths are shown below from L to R: the L superior intercostal vein, the L SVC, the L internal mammary vein, L partial anomalous pulmonary venous drainage and the L pericardiophrenic vein which outlines the L heart border.
This does bring up the subject of central line complications. The overall failure rate of central lines is 10% including bloodstream infections, pneumothorax, occlusions and dislodgement. Less usual complications include pericardial tamponade, cardiac arrest from arrhythmias and aortic placement requiring sternotomy.
Of 1892 central lines in a secondary analysis of a randomized trial done in Australia, several things were found. They included 43% non tunneled lines, 40% PICs,and 17% tunneled central lines. They found:
1. Antimicrobial nontunneled CVADs were associated with significantly fewer central line–associated bloodstream infections than were other CVADs .
2. Catheters were most often dislodged during transport.
3. Midlevel lines placed with ultrasound were the safest lines.
4. Their study suggested that central lines, if placed in the ED, should be midlevel lines.
Our patient had no cardiac abnormalities and the line did not enter the L atrium so it remained in placed. She recovered from influenza induced respiratory failure and was discharged.
If you are uncertain where your line is located; you can do a blood gas or a CT OR look at the chart below.
Coentrao L, Roncon-Albuquerque, Reis P ,et al. Cardiac arrest after left subclavian venous catheter insertion. Intensive Care Medicine 2014 .40:1367-68.
Calderron A, Can we extend the replacement interval of infusion sets for indwelling vascular catheters?
Corley A et al. Incidence and risk factors for central venous access device failure in hospitalized adults: A multivariable analysis of 1892 catheters. J Hosp Med 2024 Oct ;19:905. (https://doi.org/10.1002/jhm.13414)
Journal Watch Hospital Medicine N Engl J Med 29 Oct 2024.
Chasen M, Charnsangavej C. venous chest anatomy: clinical implications. European Journal of Radiology vol 27(1)
Azizova A, Onder O, Arslan S, etla l. Persistent left superior vena cava: clinical importance and differential diagnoses