A 73 y.o. woman with a hx of stroke, comes in with altered mental status
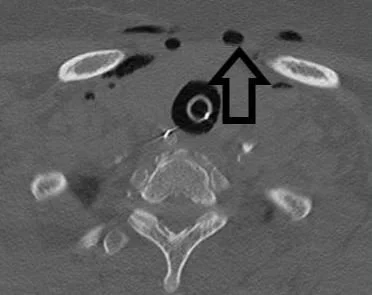
she is intubated and scanned. What do you see?
hint: there is air where it does not belong
Our patient had an air embolus caused by IV insertion
air appears similar to the air in the trachea
Air embolism is an often misdiagnosed and potentially fatal condition. Significant air embolus occurs most frequently with otolaryngological and neurosurgical procedures, barotrauma and invasive vascular procedures where the patient is on a pump. The reason air embolus is greater in ENT/neurosurgical procedures is that the incision is higher than the heart and negative pressure will allow air to enter veins especially if surgery is done in an upright position.
While significant air embolus is most common in surgical procedures, air emboli have been reported with insertion or removal of IV catheters with an incidence of 1 in 47 . So this becomes a problem most of us will see in the ED. Most of these emboli are small but if the amount is close to 50 cc; it is fatal. The air creates an air lock -effect in the main pulmonary artery trunk and results in acute right ventricl outflow tract obstruction, severe hypoxia and death.
Occasionally , the air embolus can cause an increase in R sided pressure and travel through a patent foramen into the systemic circulationan through a patent foramen ovale. If this happens a stroke or mesenteric ischemia can result.
air embolus can be seen on echo
SITUATIONS WHERE THERE IS A RISK FOR AIR/GAS EMBOLUS
Deep-sea diving-can result in nitrogen accumulating in the blood as the diver ascends.
Cardiac surgery – where the patient is on bypass
ENT surgery- where the patient is upright
GYNE surgery- especially during c section, but can occur in laparoscopy or hysteroscopy
Trauma-blunt trauma where damage to a vein allows air to enter. This can happen in lung biopsies as well.
Hydrogen peroxide ingestion- causes widespread embolism of oxygen bubbles
air embolus after hydrogen peroxide ingestion
In the cases of small amounts of venous air, it is broken down in the capillary bed without sequelae. If it enters the arterial circulation 1-2 cc can be fatal . The history is critical and temporal relationship to an invasive procedure is the biggest clue in making the diagnosis. Loss of consciousness or hemodynamic instability can result immediately. Air may be visualized in the heart on US. While positioning in the left lateral decubitus position may be beneficial to trap emboli in the R heart for removal with a central catheter, there is no data supporting the placement of an intravenous catheter for venous gas embolism management if one is not already in place Hyperbaric exygen is commonly used in arterial gas embolism.
Our patient was seen by ENT to rule out trauma secondary to intubation or NG placement. She never developed subq air and her venous gas gradually resolved. Her gas embolus was felt secondary to IV insertion. She remains hospitalized for seizures
Barzalai I, Braden G, Ford L. et al. Renal angiomyolipoma with arteriovenous shunting Case Resports J Urol. 1987 Mar;137(3):483-4.
Mills M, Nguyen J, Jarosz S, et al. Radiol Case Rep 2018 Oct;13(5):982-87Hendriksen S, Menth N, Westgard B, et al. Hyperbaric oxygen therapy for the prevention of arterial gas embolism in food grade hydrogen peroxide ingestion. Am J Emerg med 2017 May;35(5):809.e5-809.e8. epub 2016 Dec 14.
Vinan-Vega M, Rahman M, Thompson J, et al. Air embolism follwing peripheral intravenous access. Proc(Bayl Univ Med Cent) 2019 Jul;32(3):433-434.
Gordy S, Rowell S. Vascular air embolism. Int J Crit Illn Inj Sci 2013 Jan-Mar ;3(1):73-76.
Ji J, Tiari Y, chen L, Bingbinb L. Intraoperative venous air embolism in the non-cardiac surgery-the role of perioperative echocardiography in a case series report. Ann Transl Med. 2020 June;8(12):798.