A 59 y.o. woman presents with painful swallowing and a blistering rash.
What would be a unifying diagnosis?
R leg
Left leg
Our patient had epidermolysis bullosa . this is a blistering skin condition caused by a defective keratin in the skin surface. Over 90% of the cases are epidermolysis bullosa simplex. It affects the hands and feet and is inherited as an autosomal dominant affecting keratin genes KRT5 and KRT 14. It can also affect the connections between the endoderm and underlying tissues, leading to esophageal strictures and squamous cell cancer.
BLISTERING SKIN DISEASES
1.Immune mediated-
bullous pemphigoid is the most common immunobullous disease and it affects the elderly . There is a breakdown of subepidermal tissue leading to large bullae.
Pemphigus vulgaris is potentially fatal. It often presents with oral ulcerations followed by widespread loss of skin. It is common in middle aged patients for the Indian subcontinent.
Pemphigus may be precipitated by drugs like captopril, enalapril and penicillamine. It is sometimes found in association with lymphoma or bronchogenic carcinoma.
Dermatitis herpetiformis is an IgA mediated immune blistering disease. It is associated with gluten sensitivity.
porphyria cutanea tarda
2. Liver associated-
Porphyria Cutanea tarda- is a blistering disease caused by a defect in a liver enzyme uroporphyrinogen decarboxylase. It is often found in alcoholics with liver disease. It occurs in sun exposed areas.
3. Infectious-
Impetigo is a common blistering skin infection in children caused by Staphylococcus.
Staphylococcal scalded skin syndrome- is a blistering skin condition caused by Staph infection. It is more common in summer and fall.
Varicella zoster/herpes virus – can cause blistering
Varicella in an immunocompetent patient can rarely be very severe as shown above.
Toxic epidermal necrolysis – is a blistering skin condition which can involve mucous membranes. It is usually drug related. There is a spectrum from Stevens Johnson to generalized skin loss. It is a potentially life-threatening disorder which can result in GI hemorrhage and ocular abnormalities.
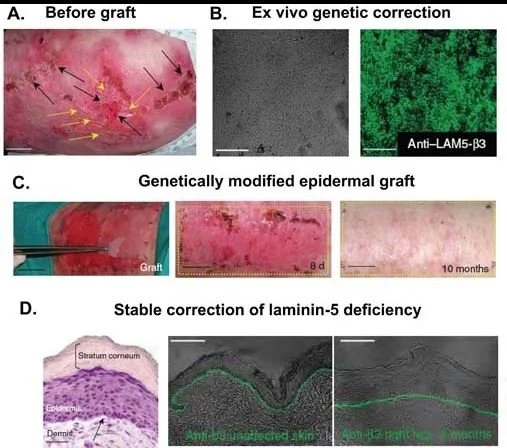
Skin grafts have been attempted to treat epidermolysis bullousa with skin modified by transplantation of laminin 5 modified stem cells. Bone marrow transplants have been done at the University of Minnesota but the immune suppression required has reported in death in four cases where there was skin breakdown and bacterial infection.
Our patient is being schedules for endoscopy to determine if she has a stricture. Her wounds are being managed with a barrier cream.
Pfendner E, Lucky A. Junctiional epidermolysis bullosa. GeneReviews Feb 22,2008.
Welsh B. Blistering skin conditions. Aust FamPhysician 2009Jul;38(7):484-90.
Mansouri S, Mai S, Hassam B, Benzekri L. Bullous varicella in an immunocompetent infacnt. BMJ Case Reports. Vol 12 Issue 3 http://dx.doi.org/10.1136/bcr-2018-229025