A 15 y.o. woman comes in with shortness of breath
What do you think is wrong?
Our patient was confirmed as having covid on a bronchoalveloar lavage after two negative covid tests. The diagnosis was finally made because of high clinical suspicion on the part of the clinician, persistently normal white blood counts, lymphopenia, and an elevated ddimer.
It is not surprising that the initial tests for covid were negative. A study from China, Wang, et al. showed that in 205 covid patients bronchoalveolar lavage showed the highest positive rates with 14 of 15 being positive at 93%, followed by sputum (72 of 104;72%), nasal swabs 5 of 8; 63%) fibrobronchoscopic brushings and biopsy (6 of 13 ; 46%), pharyngeal swabs 126 of 398;32%), feces (44 of 153;29%), blood (3 of 307);1%, and urine ( no tests positive).
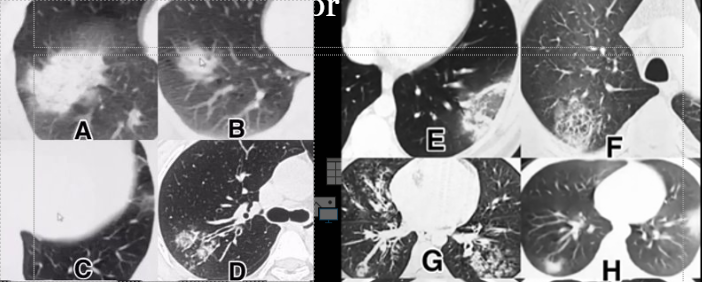
A collection of covid + patient CTs from China
Interestingly, imaging has no specificity for the diagnosis of covid with up to 50% of patients having normal CT scans initially. In populations with a high clinical suspicion and symptoms the specificity of CT scanning is 25% and sensitivity is 97%. Below are various presentations of covid on ct which look exactly like bacterial pneumonia (A and B), bronchiectasis (C and D), peripheral infarcts( E and F) and viral pneumonia (G and H). These images are shown below. To clean a CT scanner, the room should be blocked one hour prior to cleaning and the HVAC sirculate the room 6 times, then the room can be cleaned. The ED scanners have shared ventilation so patients should be done on the second floor. The process takes two hours.
The ddimer has been noted to be above 2,000 in many covid patients that are going to decompensate which may be a sign that they are going in to a cytokine storm.
A recent Dutch study from April 10 found 35% of covid patients had blood that clotted abnormally despite thrombosis prophylaxis. Autopsies have shown some people’s lungs are filled with hundreds of microclots leading some centers to heparinize all covid patients. If the fibrinogen is high it is thought that low molecular weight heparin should be used for anticoagulation because unfractionated heparin gets used by the massive amount of fibrinogen and the pt never gets therapeutic. The clotting phenomenon appears to be new in this virus since Ebola, dengue and other hemorrhagic fevers lead to bleeding not clotting. Clotting may also explain why pregnant patients are at risk for sudden death. Our patient was pregnant and she was delivered but remains in the ICU.
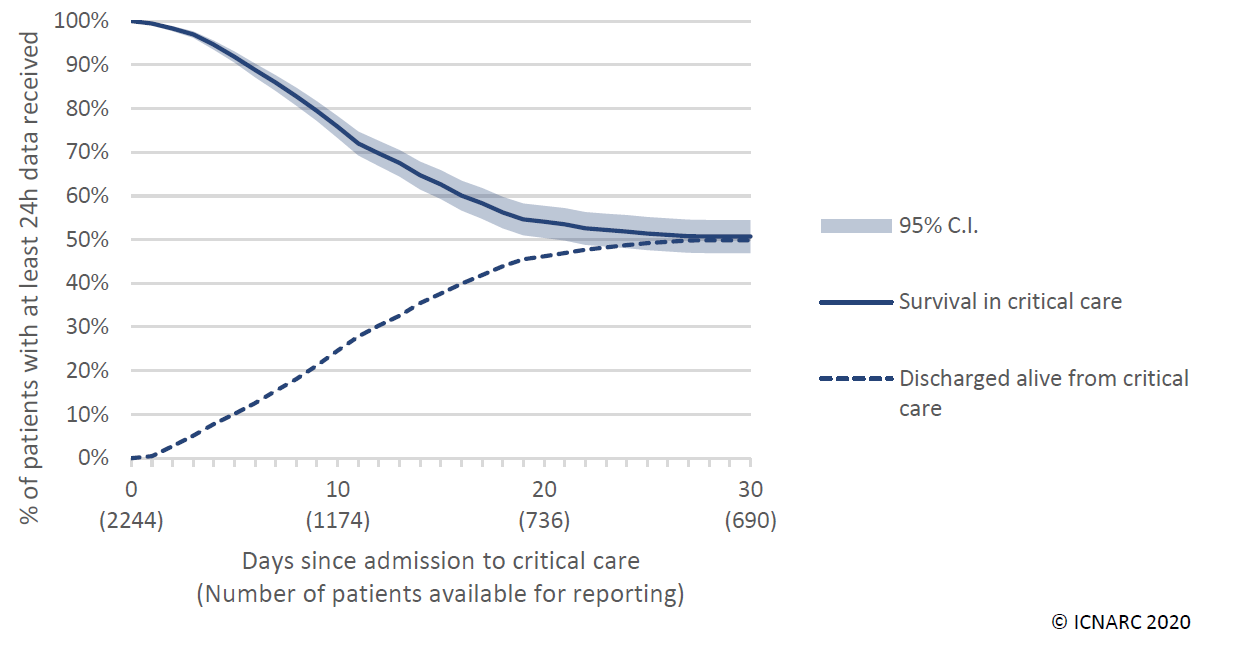
30 day survival in the UK
It appears the virus has been circulating much longer than the first death reported in Washington state Feb 29. Autopsies in California reported on post mortem testing confirmed a case Feb 6 and one Feb 17. Both died in Santa Clara county where the recent antibody testing showed many more people have antibodies than ever reported symptoms.
As regards antibody testing; the IgM is thought to be present in about 8 days and the IgG( which some are touting as a sign of immunity) takes 20 days to develop. The CDC has approved only four tests as of April 4, but the FDA just approved an at home test kit. It’s the Wild West out there now with multiple vendors advertising tests. Caveat emptor!
Thanks to Drs. Bierhals and Osborn.
Wang, W, Xu Y, Gao R, et al. JAMA march 11, 2020, published on line doi:10.1001/jama.2020.3786.
COVID-19@icnarc.org ( report from the National Health Service), reports all cases reported to the National Health Service. April 4 2020.
Klok F, Kruip M, van der Meer N, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thrombosis Research, April 2020, https://doi.org/10.1026/j.thromres. 2020.04.013