A 78 y.o. male on hemodialysis with a hx of cirrhosis and monthly paracentesis presents with abdominal pain
what do you notice?
the pt is hypotensive; what needs to be done?
Our patient had a large abdominal abscess, walled off from the rest of his ascites four days after his last paracentesis. Interventional placed drains as he was deemed not to be a surgical candidate; He grew out mixed anaerobes presumably from a bowel perforation. He became septic and inspite of heroic measures; died from this infection.
The word paracentesis comes from a Greek word meaning “to puncture”. Since paracentesis is more effective for the treatment of ascites than diuretics it is often done, even in the ED.
How common is a complication after paracentesis?
It is estimated the rate of minor complications is 10%. This includes leakage of ascites, failure to drain ascites, hypotension, or infection.
The risk of major complications is estimated at 1.6% which includes venous bleeding requiring transfusion. hepatorenal syndrome, arterial bleeding or bowel perforation. Risk of bleeding increased with INR > 1.6 and platelet count of < 50,000. Risk of bleeding can be mitigated by the use of ultrasound in selecting the site of the procedure.
AVOID COMPLICATIONS
--Use ultrasound to avoid major vessels.
inferior epigastric vessels
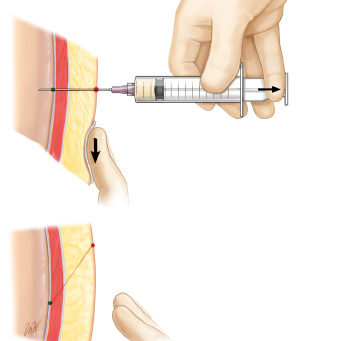
--Use a Z track insertion to prevent leakage
the skin is pulled down as the lidocaine is injected and when it is released the abdominal wall helps retain ascitic fluid
__ Give albumin in large volume paracentesis to prevent hypotension and hepatorenal syndrome . If 4-5 L are removed 6-8 gm/L of 25% albumin should be given.
Sudulagunta S, Sodalagunta M, Raja S, et al. Clinical profile and complications of paracentesis in refractory ascites patients with cirrhosis. 2015 Gatroenterology Res. Aug;8(3-4):228-233.
Gines P, Cardenas Arroyo V, rodes J. Management of cirrhosis and ascites. N Engl J Med 2004;350(16):1646-1654.
Runyon B. Paracentesis of ascetic fluid. A safe procedure. Arch Intern med 1986;146(11):2259-2261.
https://www.uptodate.com/contents/diagnostic-and-therapeutic-abdominal-paracentesis
ASCITES REVIEW
A TIPS bypasses the cirrhotic liver
The chief factor contributing to ascites is increased hepatic resistance to portal flow due to cirrhosis. This causes portal hypertension, collateral vein formation and shunting of blood to the systemic circulation. As portal hypertension develops nitric oxide is produced and splanchnic arterial dilation occurs so blood volume decreases and arterial bp falls. As bp falls sodium is retained and fluid accumulates in the abdomen. Severe constriction of renal circulation can occur with oliguria and the hepatorenal syndrome.
A transjugular intrahepatic portosystemic shunt(TIPS) can be inserted between the hepatic vein and portal vein to decrease portal hypertension but it causes the risk of hepatic encephalopathy.