An elderly patient on peritoneal dialysis with abdominal pain...
You are working one evening when an elderly gentleman is sent in by his nephrologist for abdominal pain. The patient has a history of renal failure and is on peritoneal dialysis. Last evening, he developed sudden, severe abdominal pain and was unable to perform PD at home. Today, he went to the outpatient dialysis unit where they withdrew some fluid. His nephrologist ordered a CT of the abdomen and pelvis which demonstrated the following:
The patient's VS are the following:
T 97.5 P 94 RR 18 BP 174/97 Sat 98% on RA
What is your differential diagnosis? What would you do next?
Scroll down for the case conclusion.
Final diagnosis: Iatrogenic pneumoperitoneum from injection of air through peritoneal dialysis catheter
Case Conclusion: The patient was noted to have a large amount of free air on his CT scan (which was actually a CT peritoneogram in which contrast was injected into the peritoneum via the PD catheter, thereby accounting for contrast in the peritoneal space). The air was evacuated from his peritoneum via the dialysis catheter and his pain improved. An upper GI series performed with water-soluble contrast was negative for perforation. The patient was admitted for serial abdominal exams and discharged to home the next day. It was determined that the patient likely had inadvertently allowed air to enter his peritoneum via the PD catheter and he was re-instructed on proper technique.
Learning Points:
On a broader scale, the differential diagnosis for abdominal pain in a patient on peritoneal dialysis includes both the regular causes of abdominal pain (e.g. bowel obstruction, diverticulitis, mesenteric ischemia etc.) as well as the complications of the peritoneal dialysis catheter itself [1]. Peritoneal dialysis catheter complications that need to be considered include:
Infection. The most common complication in PD patients is bacterial infection causing peritonitis.
Catheter failure. This may be due to malposition, kinking or entrapment. Interestingly, adhesions from prior episodes of peritonitis are the most frequent cause of maldistribution of dialysate, which can cause dialysis failure and intestinal obstruction.
Hernias. Hernias are seen in up to 25% of PD patients due to a combination of raised intrabdominal pressure and a peritoneal defect caused by catheter insertion.
Dialysate leaks. These may be at the site of catheter insertion due to a tear in the peritoneum; however, dialysate can also leak into the thoracic cavity (via pleuroperitoneal connections), scrotum (via the processus vaginalis), and the retroperitoneum.
Encapsulating sclerosing peritonitis. This is a relatively rare inflammatory process occurs in ~ 1 % of PD patients. It leads to the deposition of a thick fibrous membrane in the peritoneum, causing ultrafiltration failure and potential bowel complications.
…. and iatrogenic pneumoperitoneum
The finding of pneumoperitoneum in any patient must prompt concern for a perforated viscus. However, as the great orator Robert Ingersoll once said:
This can be translated into modern day emergency medicine by saying:
"The patient’s presentation is the product of all their past medical history and procedures, which is the necessary cause of their future management and disposition."
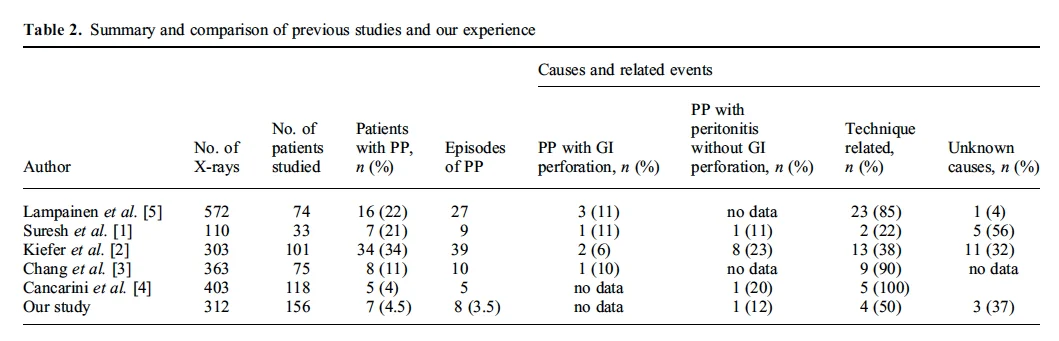
While the most common way to get air into the peritoneum is by perforating a viscus, the presence of a peritoneal dialysis (PD) catheter allows for an additional portal of air into the peritoneum. The incidence of pneumoperitoneum in patients on PD presenting to the hospital for a myriad of complaints ranges from 4-35% [2]. In the majority of cases, the pneumoperitoneum is due to poor technique and introduction of air into system during bag changes (see Table 2 below).
Source: Reference 2
However, anywhere from 6-11% of the patients with pneumoperitoneum have a perforation [2]. Therefore, the possibility of a gastric or bowel perforation needs to be strongly considered in the presence of pneumoperitoneum. In this patient with stable vital signs and significant improvement in pain with evacuation of air, viscous perforation would be much less likely and further imaging/observation an appropriate course of action.
Case Conclusion by Maia Dorsett (@maiadorsett)
References:
1. Goldstein, M., Carrillo, M., & Ghai, S. (2013). Continuous ambulatory peritoneal dialysis—a guide to imaging appearances and complications. Insights into imaging, 4(1), 85-92.
2. Imran, M., Bhat, R., & Anijeet, H. (2011). Pneumoperitoneum in peritoneal dialysis patients; one centre’s experience. NDT plus, sfq208.