EKG Challenge No. 15 Case Conclusion: Too Much Ibuprofen?
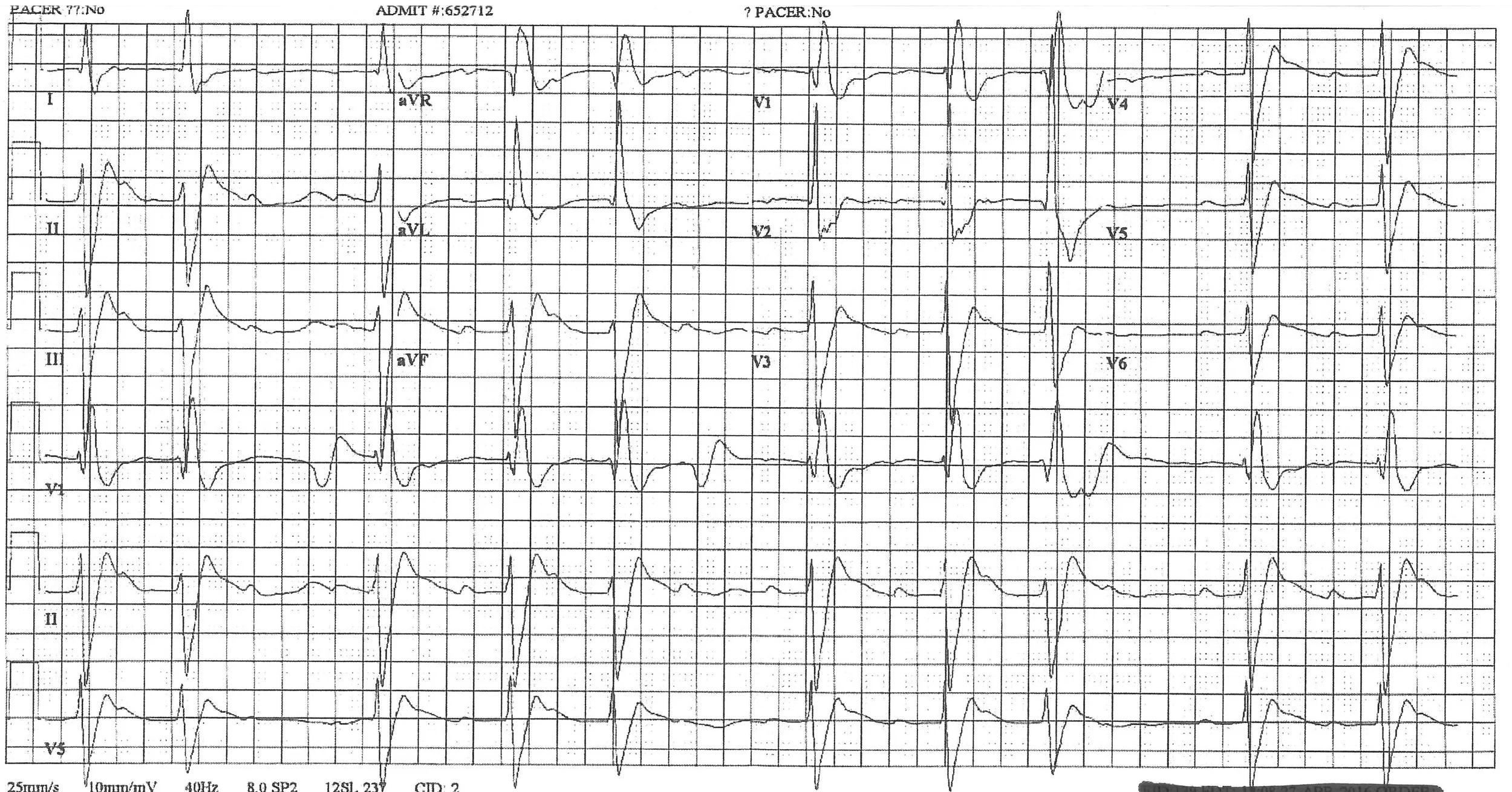
Paramedics bring in a 29 year old male with a history of depression and alcohol abuse for a reported ibuprofen ingestion of unknown quantity as a suicide attempt. The patient initially was somnolent and admitted to alcohol use, but while being transported suddenly had a generalized tonic-clonic seizure. Paramedics quickly administer IV diazepam for the resolution of seizure activity, and he is post-ictal on arrival to the ED. Blood pressure is 98/60 with an irregularly irregular heart rate of 62 on the monitor. He has no history of seizures or cardiac disease in his records. His 12-lead EKG shows this:
The EKG machine read this as "Sinus bradycardia with 1st degree A-V block with premature supraventricular complexes, right bundle branch block, left anterior fascicular block, left ventricular hypertrophy with QRS widening and repolarization abnormality." Great. But this makes no sense--an ibuprofen overdose doesn't cause EKG changes like this. SOMETHING is missing in the history!
Most concerning on this EKG are the intraventricular conduction delay (widened QRS) and the prominent R' in aVR, which should raise your suspicion for sodium channel blockade. It was discovered later by family that there was an empty 100 tablet bottle of 50 mg diphenhydramine tablets at the house that was full just a few days prior.
Diphenhydramine is a commonly available drug used for allergic reactions, colds, and as a sleep aid. With mild overdoses, diphenhydramine will cause sedation and anti-cholinergic effects (dry mucous membranes, hot flushed skin, mydriasis, urinary retention, tachycardia). Higher doses can result in central nervous system toxicity, including agitation, delirium, seizures and even coma. Large overdoses of diphenhydramine can also cause significant sodium-channel blockade similar to class 1a anti-arrhythmics [1], which lead to the above EKG findings. This can be seen in tricyclic antidepressant overdoses also, as there is a similar mechanism of sodium channel blockade, and includes QRS prolongation (QRS > 100 ms) and prominent terminal R waves in aVR (R' > 3 mm) [2].
EKG in a patient with a tricyclic antidepressant overdose. The QRS duration here was 122 ms. Note the tall R' in aVR, which is more subtle than the diphenhydramine overdose EKG above.
So what to do if you come across this overdose patient with severe, life-threatening diphenhydramine overdose? In addition to stabilizing airway, breathing, and circulation, your next step should be administering sodium bicarbonate IV, which should help narrow the QRS and ward off ventricular dysrhythmias and seizures. Serial EKGs should be checked after sodium bicarbonate infusion (e.g. 2 mEq/kg or 150 mEq of sodium bicarbonate), and if the QRS still is > 100 ms then sodium bicarbonate should be repeated. If the EKG remains unchanged, the use of IV lipid emulsion therapy is an option supported by a few case studies [1,3]. Consultation with a medical toxicologist or poison control center should be sought for cases with severe toxicity.
Patient Follow Up
In the ED, the patient was treated with sodium bicarbonate but unfortunately and quickly had worsening hypotension refractory to pressors and went into cardiac arrest. Despite a prolonged resuscitation, the patient ultimately did not survive.
Summary
- Never trust your overdose patients and rule out other potential ingestions with an EKG, acetaminophen level, and salicylate levels.
- Classic signs of sodium channel toxicity (diphenhydramine, tricyclic antidepressants, anti-arrhythmic overdoses) include
- QRS prolongation > 100 ms
- Tall R' wave in aVR
- Treat sodium channel toxicity with sodium bicarbonate and consider IV lipid emulsion therapy in refractory cases
Submitted by Phil Chan (@PhilChanEM), PGY-3
Faculty reviewed by David Liss (@dave_liss), Toxicology Fellow
References
1) West J Emerg Med. 2014;15(7):855–858.