EKG Challenge No. 13 Case Conclusion: Sometimes The Pain Ain't From Cocaine
You are working one evening in the emergency department when you walk
in to see your 4th chest pain patient of the night. Your current
patient is a 50-something year old male who's years of homelessness and
cocaine abuse have made him appear older than his stated age. He tells
you that he has been having left sided chest pain on and off for the
last 3 hrs. He received ASA and nitro x 2 in the ambulance and now
feels much better. You examine his EKG from today:
You then compare it to his EKG from two days ago when he came in for chronic diarrhea (and had mentioned some intermittent chest pain):
... and compare it again with his EKG from 1 year before during an admission for chest pain in which he had a negative cardiac stress test:
Initially, you compare his first and second EKG. You think, "those T waves in V2 and V3 look weird, but they are unchanged from previous". However, you note that this prior EKG was only a couple days before and you compare them with the EKG from a year before... when those strange, biphasic T waves were not present.
Whenever you see T wave abnormalities in a patient with possible unstable angina, you need consider an electrocardiographic syndrome of critical LAD stenosis that was first described by Hein Wellens and colleagues in 1982 and thus is referred to as Wellen's Syndrome.
Wellens' Syndrome is a clinical-electrocardiographic syndrome with the following criteria [1,2]:
- Prior history of chest pain - i.e. the patient is now chest pain free
- Little or no cardiac enzyme elevation
- No pathologic precordial Q waves
- Little or no ST-segment elevation
- Symmetric or deeply inverted T waves in leads V2 and V3 (and occasionally the other precordial leads as well) OR biphasic T wave in leads V2 and V3
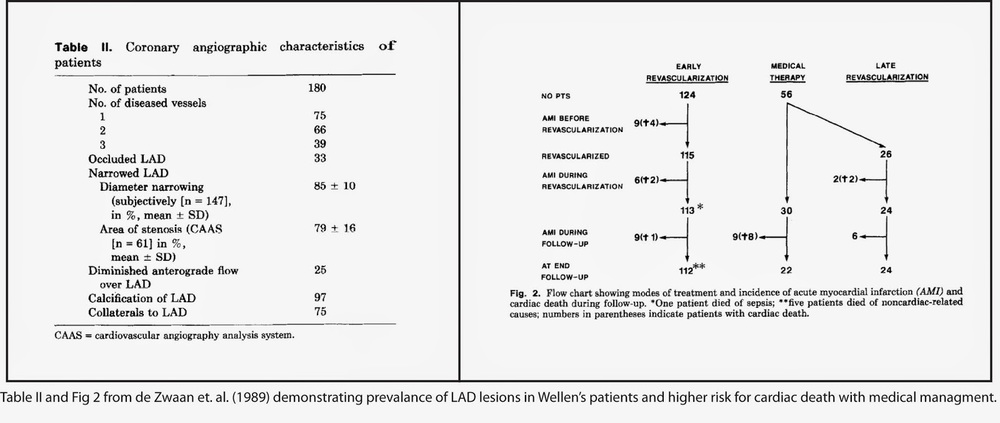
As noted above, Wellens' syndrome has variable electrocardiographic presentations. It comes in one of two forms: symmetric, deep T wave inversions (75% of cases) or biphasic T waves (25% of cases) [2,3]. These T wave inversions are notable for their steep angle of descent and depth. While changes in V2, V3 are typical, T-wave abnormalities may also be present in the other precordial leads (V1, V4, V5, V6) as well. Wellens' syndrome is dynamic, which is one of the features that distinguishes it from more benign causes of precordial T wave inversion such as LVH with strain. Dr. Steve Smith's ECG blog has this post on distinguishing benign T wave inversion from Wellens' syndrome.
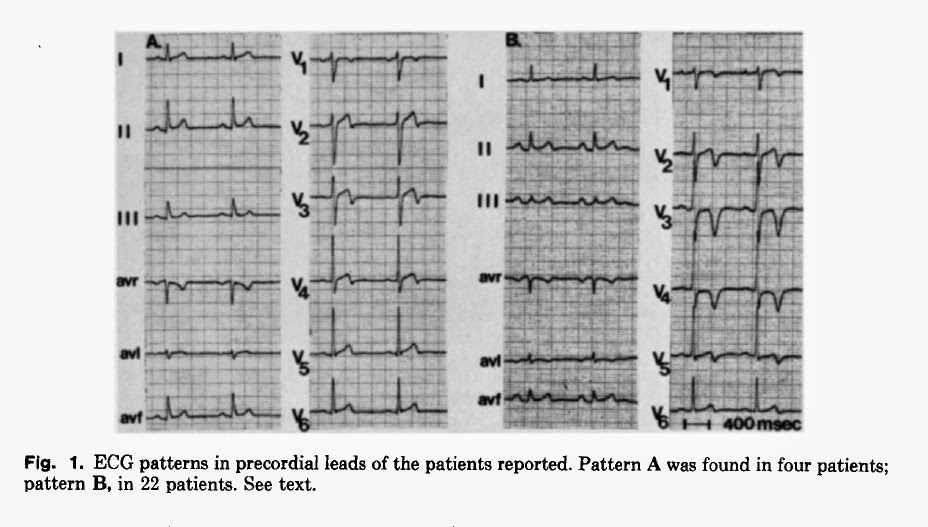
Wellens' syndrome was first identified by a retrospective study of patients presenting with unstable angina [3]. This study found a strong correlation between one of two distinct patterns of T wave abnormalities in V2 and V3 and high risk for progression to large anterior wall myocardial infarction. This association was re-confirmed with a follow-up prospective study of 204 patients admitted to their hospital between 1980-1985 with unstable angina and findings of Wellens' syndrome on the EKG. 180 of these patients underwent cardiac catheterization. All had evidence of LAD lesions, 29% of which were proximal to the first septal perforator. In general, patients who had medical management vs. angioplasty were more likely to die of sudden cardiac death (8/30 for medical management vs. 3/115) [4].
Given the high risk of progression to left anterior wall myocardial infarction and death, patients with Wellens' syndrome should NOT undergo a cardiac stress test. [2] They should go cardiac catheterization sooner rather than later (probably from the ED in ideal circumstances) as they are extremely high risk for progression to anterior STEMI:
After intervention and with time, ninety percent of patients with Wellens' syndrome will regain a normal ST-T segment [4]. While an exact time period for resolution of EKG changes was not specified in Wellens' paper, ST-T wave abnormalities were more likely to persist in patients who continued to have chest pain, undergo medical therapy, or had extensive collateral circulation on cardiac catheterization suggesting longer term and more permanent cardiac injury.
So what happened with our patient? After his second presentation with unstable angina and biphasic T waves, the emergency physician diagnosed him with Wellens' syndrome and admitted him to the Cardiology service where he was taken for cardiac catheterization and underwent stenting of a 90% lesion in his proximal LAD. While his hospital discharge summary announced that "it was felt that his chest pain was still most likely to costochondritis or cocaine use", the change in T wave morphology on his post-cath EKG suggests otherwise:
Clinical Take Home: Proper risk stratification and correct disposition of patients presenting with possible acute coronary syndrome is a common and difficult problem faced by pre-hospital personnel and emergency physicians. While anterior T wave abnormalities can have a wide differential diagnosis with both benign and concerning causes [including but not limited to persistent juvenile T wave inversion, pulmonary embolism, ongoing cardiac ischemia and neurocardiogenic injury], in a now pain free patient with symptoms of unstable angina a critical LAD stenosis with high risk for progression to large anterior wall MI must be considered. These patients should undergo cardiac catheterization sooner rather than later as they are at very high risk for progression to massive acute anterior wall myocardial infarction. Do not under any circumstances send them for a stress test, as this may trigger massive MI and cardiac arrest. Finally, be a patient advocate. Although coronary vasospasm from cocaine use can cause a pseudo-Wellens' syndrome, this is a diagnosis of exclusion. Just because a patient uses drugs does not mean that he/she does not have underlying coronary artery disease.
Submitted by Maia Dorsett (@maiadorsett), PGY-3
Faculty Reviewed by Brent Ruoff
Thank you to Julianne Dean and Chris Palmer for the cases (and patient advocacy)
References:
[1]Tandy, T. K., Bottomy, D. P., & Lewis, J. G. (1999). Wellens’ syndrome. Annals of emergency medicine, 33(3), 347-351.
[2]Rhinehardt, J., Brady, W. J., Perron, A. D., & Mattu, A. (2002). Electrocardiographic manifestations of Wellens' syndrome. The American journal of emergency medicine, 20(7), 638-643.
[3] de Zwann, C., Bar F.W., Wellens, H.J. (1982). Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction." American heart journal, 103(4), 730-736.
[4] de Zwaan, C., Bär, F. W., Janssen, J. H., Cheriex, E. C., Dassen, W. R., Brugada, P., ... & Wellens, H. J. (1989). Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. American heart journal, 117(3), 657-665.
 |
| EKG #1 (day of presentation) |
You then compare it to his EKG from two days ago when he came in for chronic diarrhea (and had mentioned some intermittent chest pain):
 |
| EKG #2 (EKG from two days prior to presentation) |
... and compare it again with his EKG from 1 year before during an admission for chest pain in which he had a negative cardiac stress test:
 |
| EKG #3 (EKG from one year prior to presentation) |
Whenever you see T wave abnormalities in a patient with possible unstable angina, you need consider an electrocardiographic syndrome of critical LAD stenosis that was first described by Hein Wellens and colleagues in 1982 and thus is referred to as Wellen's Syndrome.
Wellens' Syndrome is a clinical-electrocardiographic syndrome with the following criteria [1,2]:
- Prior history of chest pain - i.e. the patient is now chest pain free
- Little or no cardiac enzyme elevation
- No pathologic precordial Q waves
- Little or no ST-segment elevation
- Symmetric or deeply inverted T waves in leads V2 and V3 (and occasionally the other precordial leads as well) OR biphasic T wave in leads V2 and V3
As noted above, Wellens' syndrome has variable electrocardiographic presentations. It comes in one of two forms: symmetric, deep T wave inversions (75% of cases) or biphasic T waves (25% of cases) [2,3]. These T wave inversions are notable for their steep angle of descent and depth. While changes in V2, V3 are typical, T-wave abnormalities may also be present in the other precordial leads (V1, V4, V5, V6) as well. Wellens' syndrome is dynamic, which is one of the features that distinguishes it from more benign causes of precordial T wave inversion such as LVH with strain. Dr. Steve Smith's ECG blog has this post on distinguishing benign T wave inversion from Wellens' syndrome.
 |
| Figure 1 from the original paper describing Wellens' syndrome (Ref 3). Note the two patterns of precordial T wave abnormalities. |
Given the high risk of progression to left anterior wall myocardial infarction and death, patients with Wellens' syndrome should NOT undergo a cardiac stress test. [2] They should go cardiac catheterization sooner rather than later (probably from the ED in ideal circumstances) as they are extremely high risk for progression to anterior STEMI:
 |
| Figure 2 from the original paper demonstrating progression from Wellens' to STEMI (and death). |
After intervention and with time, ninety percent of patients with Wellens' syndrome will regain a normal ST-T segment [4]. While an exact time period for resolution of EKG changes was not specified in Wellens' paper, ST-T wave abnormalities were more likely to persist in patients who continued to have chest pain, undergo medical therapy, or had extensive collateral circulation on cardiac catheterization suggesting longer term and more permanent cardiac injury.
So what happened with our patient? After his second presentation with unstable angina and biphasic T waves, the emergency physician diagnosed him with Wellens' syndrome and admitted him to the Cardiology service where he was taken for cardiac catheterization and underwent stenting of a 90% lesion in his proximal LAD. While his hospital discharge summary announced that "it was felt that his chest pain was still most likely to costochondritis or cocaine use", the change in T wave morphology on his post-cath EKG suggests otherwise:
Submitted by Maia Dorsett (@maiadorsett), PGY-3
Faculty Reviewed by Brent Ruoff
Thank you to Julianne Dean and Chris Palmer for the cases (and patient advocacy)
References:
[1]Tandy, T. K., Bottomy, D. P., & Lewis, J. G. (1999). Wellens’ syndrome. Annals of emergency medicine, 33(3), 347-351.
[2]Rhinehardt, J., Brady, W. J., Perron, A. D., & Mattu, A. (2002). Electrocardiographic manifestations of Wellens' syndrome. The American journal of emergency medicine, 20(7), 638-643.
[3] de Zwann, C., Bar F.W., Wellens, H.J. (1982). Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction." American heart journal, 103(4), 730-736.
[4] de Zwaan, C., Bär, F. W., Janssen, J. H., Cheriex, E. C., Dassen, W. R., Brugada, P., ... & Wellens, H. J. (1989). Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. American heart journal, 117(3), 657-665.