EKG Challenge No. 7 Case Conclusion - Not Everything is a Medical Mystery
A 22-year-old female with no past medical history presents to the
Emergency Department after a syncopal episode at home. She reports
feeling lightheaded and then noticed her heart was pounding, prior to
passing out. Her mother caught her, and she came to in "about a minute."
She was brought to the ED by EMS. On further history, she stated she
had not eaten anything today and had just gotten back from a jog outside
when she began to feel lightheaded. She had a few similar episodes in
the past when she has had blood drawn. Now she feels slightly weak but
otherwise back to normal. Fingerstick glucose is normal, as well as CBC,
BMP, and U/A. Her pregnancy test is negative. Her EKG is below.

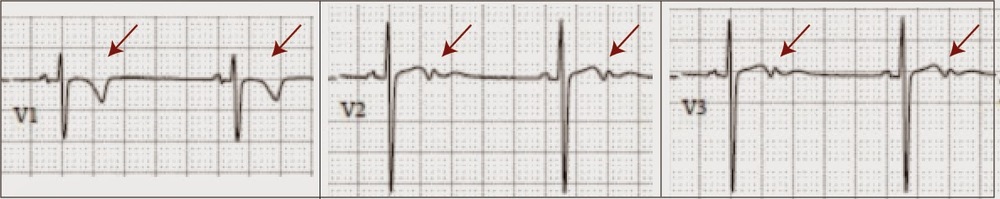
You review the EKG and are at first concerned about the T wave abnormalities in the V1 - V3. Your colleague (ahem, attending) then looks over your shoulder and states, "well looks like she might have persistent juvenile T wave inversion".
Persistent Juvenile T wave Inversion is a benign finding found predominantly in young females [1, 2]. Prior to birth, the right heart must pump against high pulmonary pressures, causing it to be thicker and stronger than the pediatric left heart. Pediatric EKGs often reflect this with right axis deviation and anterior t-wave inversion. Right axis deviation should resolve before early adolescence, but in some individuals the pattern of precordial T wave inversion persists (hence the name). The EKG findings of Persistent Juvenile T wave inversion? Per Amal Mattu (see Mattu's ECG case of the week and Ref 3]:
Shallow and asymmetric T wave abnormalities in V1-V3 (either inversions or biphasic T waves).
From our patient:
Is there any clinical significance to persistent Juvenile T wave inversion and is there anything that we should do about it? The answer is probably no. A recent Finnish study [4] recorded EKGs of 10,000 middle-aged patients and then collected morbidity and mortality data for 30 years. 0.5% of patients were found to have anterior t-wave inversion on their baseline EKG. No adverse outcomes were associated with anterior t-wave inversions. A Turkish study [2] evaluated the correlation between anterior T wave inversions in adulthood and risk factors for cardiovascular disease. No correlation was found in male subjects (where anterior T wave inversions were rare), but women with anterior T wave inversions were more likely to have a lower SBP and a higher incidence of Type 2 Diabetes. It is unclear whether these findings have any clinical significance or are the product of a shotgun approach to identifying correlations. However, an Italian study [5] of nearly 3000 peri- and post-pubertal children (age range 8-18) found t-wave inversion to be present in 158 (5.8%), with a significant decline after puberty. These children underwent echocardiography and 4 were diagnosed with cardiomyopathy [including arrhythmogenic right ventricular cardiomyopathy (n=3) and hypertrophic cardiomyopathy (n=1)]. This study recommended further testing for post-pubertal patients with persistent anterior t-wave inversion.
Our patient? She was diagnosed with vasovagal syncope and was discharged to home. This was likely an appropriate disposition given the clinical history (although some would have considered an echo per the studies above), which brings up an important point:
Always interpret the EKG within the clinical context.
If this EKG had been obtained because of high clinical suspicion for ischemia or pulmonary embolism, the precordial T wave inversions would be significantly more concerning. As an emergency physician, it is important to be aware of the differential diagnosis and implications for different T wave morphologies.
In the context of chest pain, precordial biphasic t-waves can be concerning in adult patients, particularly in the setting of chest pain [3]. T wave changes can be associated with ischemia or infarct. In ACS, the T-waves are classically symmetric and concave (see Figure blow) and in contrast to persistent juvenile T wave inversion, more likely to extend to V4-V6. It is particularly important for emergency physicians and EMS providers to familiarize themselves with Wellen's syndrome, which is characterized by inverted or biphasic t-waves in leads V2-V3 [6]. Wellen's syndrome is associated with a nearly occlusive lesion in the LAD . Patients present with a history of chest pain and when the EKG is recorded during a pain free period, the anterior t-waves are seen. Cardiac enzymes may be slightly elevated or normal. If you diagnose a patient with Wellen's syndrome, Cardiology should be consulted emergently for possible catheterization. Emergency physicians should be wary of ordering stress tests for patients with chest pain, normal troponins and anterior t-wave inversion, as this could lead to complete LAD occlusion and death in a patient with Wellens syndrome.
Anterior T wave inversions are also seen in patients with pulmonary embolism, although these after often associated with T wave inversions in the inferior leads as well.
Precordial T wave inversions are also seen in the
baseline EKGs of patients prone to life threatening arrythmmias, which
may initially present as syncope. These have been previously reviewed
in a post on the can't miss EKG findings in syncope, but we will briefly touch on them here.
- Brugada syndrome [7] is characterized by RBBB and abnormal ST waves in the anterior leads, including t-wave inversion in Brugada syndrome type 1. Brugada
syndrome is associated with a mutation in a cardiac sodium channel,
which creates a variation in ventricular repolarization. There are three
types of Brugada syndrome, and each type is associated with different
t-wave morphology (see Fig). Although the exact pathophysiology is not
known, this channelopathy can also lead to sudden onset ventricular
fibrillation or tachycardia.
t-wave inversion in Brugada syndrome type 1. Brugada
syndrome is associated with a mutation in a cardiac sodium channel,
which creates a variation in ventricular repolarization. There are three
types of Brugada syndrome, and each type is associated with different
t-wave morphology (see Fig). Although the exact pathophysiology is not
known, this channelopathy can also lead to sudden onset ventricular
fibrillation or tachycardia.
- Arrhythmogenic right ventricular dysplasia [8] could also present with t-wave inversion in anterior leads. Arrhythmogenic right ventricular dysplasia (or cardiomyopathy) is characterized by fibro-fatty replacement of the right ventricular myocardium, and is associated with ventricular arrhythmias. EKG findings can include depolarization and/or repolarization changes in the right ventricular leads, including anterior t-wave inversion.
Take Home Points: Anterior t-wave inversion is common in children. In adult (females) it can be a normal variant. However, in the right clinical context, it also be associated with sudden death, PE, or myocardial ischemia, and therefore may merit further evaluation, particularly in patients with chest pain or suspicion for arrhythmia.
Submitted by Laura Wallace (@labellalaura), PGY-3
Edited by Maia Dorsett (@maiadorsett), PGY-3
Faculty Reviewed by Evan Schwarz
References:
1. Assali, A. R., Khamaysi, N., & Birnbaum, Y. (1997). Juvenile ECG pattern in adult black Arabs. Journal of electrocardiology, 30(2), 87-90.
2. Onat, T., Onat, A., & Can, G. (2008). Negative T wave in chest lead V1: relation to sex and future cardiovascular risk factors. Turk Kardiyol Dern Ars, 36(8), 513-518.
3. Hayden, G. E., Brady, W. J., Perron, A. D., Somers, M. P., & Mattu, A. (2002). Electrocardiographic T-wave inversion: differential diagnosis in the chest pain patient. The American journal of emergency medicine, 20(3), 252-262.
4. Aro, A. L., Anttonen, O., Tikkanen, J. T., Junttila, M. J., Kerola, T., Rissanen, H. A., ... & Huikuri, H. V. (2012). Prevalence and prognostic significance of T-wave inversions in right precordial leads of a 12-lead electrocardiogram in the middle-aged subjects. Circulation, 125(21), 2572-2577.
5. Migliore, F., Zorzi, A., Michieli, P., Marra, M. P., Siciliano, M., Rigato, I., ... & Corrado, D. (2012). Prevalence of cardiomyopathy in Italian asymptomatic children with electrocardiographic T-wave inversion at preparticipation screening. Circulation, 125(3), 529-538.
6. Mead, N. E., & O'Keefe, K. P. (2009). Wellen's syndrome: An ominous EKG pattern. Journal of Emergencies, Trauma and Shock, 2(3), 206.
7. Berne, P. (2012). Brugada syndrome. Circ J, 76(7), 1563-71.
8. Corrado, D., Buja, G., Basso, C., & Thiene, G. (2000). Clinical diagnosis and management strategies in arrhythmogenic right ventricular cardiomyopathy. Journal of electrocardiology, 33, 49-55.

You review the EKG and are at first concerned about the T wave abnormalities in the V1 - V3. Your colleague (ahem, attending) then looks over your shoulder and states, "well looks like she might have persistent juvenile T wave inversion".
Persistent Juvenile T wave Inversion is a benign finding found predominantly in young females [1, 2]. Prior to birth, the right heart must pump against high pulmonary pressures, causing it to be thicker and stronger than the pediatric left heart. Pediatric EKGs often reflect this with right axis deviation and anterior t-wave inversion. Right axis deviation should resolve before early adolescence, but in some individuals the pattern of precordial T wave inversion persists (hence the name). The EKG findings of Persistent Juvenile T wave inversion? Per Amal Mattu (see Mattu's ECG case of the week and Ref 3]:
Shallow and asymmetric T wave abnormalities in V1-V3 (either inversions or biphasic T waves).
From our patient:
Is there any clinical significance to persistent Juvenile T wave inversion and is there anything that we should do about it? The answer is probably no. A recent Finnish study [4] recorded EKGs of 10,000 middle-aged patients and then collected morbidity and mortality data for 30 years. 0.5% of patients were found to have anterior t-wave inversion on their baseline EKG. No adverse outcomes were associated with anterior t-wave inversions. A Turkish study [2] evaluated the correlation between anterior T wave inversions in adulthood and risk factors for cardiovascular disease. No correlation was found in male subjects (where anterior T wave inversions were rare), but women with anterior T wave inversions were more likely to have a lower SBP and a higher incidence of Type 2 Diabetes. It is unclear whether these findings have any clinical significance or are the product of a shotgun approach to identifying correlations. However, an Italian study [5] of nearly 3000 peri- and post-pubertal children (age range 8-18) found t-wave inversion to be present in 158 (5.8%), with a significant decline after puberty. These children underwent echocardiography and 4 were diagnosed with cardiomyopathy [including arrhythmogenic right ventricular cardiomyopathy (n=3) and hypertrophic cardiomyopathy (n=1)]. This study recommended further testing for post-pubertal patients with persistent anterior t-wave inversion.
Our patient? She was diagnosed with vasovagal syncope and was discharged to home. This was likely an appropriate disposition given the clinical history (although some would have considered an echo per the studies above), which brings up an important point:
Always interpret the EKG within the clinical context.
If this EKG had been obtained because of high clinical suspicion for ischemia or pulmonary embolism, the precordial T wave inversions would be significantly more concerning. As an emergency physician, it is important to be aware of the differential diagnosis and implications for different T wave morphologies.
In the context of chest pain, precordial biphasic t-waves can be concerning in adult patients, particularly in the setting of chest pain [3]. T wave changes can be associated with ischemia or infarct. In ACS, the T-waves are classically symmetric and concave (see Figure blow) and in contrast to persistent juvenile T wave inversion, more likely to extend to V4-V6. It is particularly important for emergency physicians and EMS providers to familiarize themselves with Wellen's syndrome, which is characterized by inverted or biphasic t-waves in leads V2-V3 [6]. Wellen's syndrome is associated with a nearly occlusive lesion in the LAD . Patients present with a history of chest pain and when the EKG is recorded during a pain free period, the anterior t-waves are seen. Cardiac enzymes may be slightly elevated or normal. If you diagnose a patient with Wellen's syndrome, Cardiology should be consulted emergently for possible catheterization. Emergency physicians should be wary of ordering stress tests for patients with chest pain, normal troponins and anterior t-wave inversion, as this could lead to complete LAD occlusion and death in a patient with Wellens syndrome.
Anterior T wave inversions are also seen in patients with pulmonary embolism, although these after often associated with T wave inversions in the inferior leads as well.
 |
- Brugada syndrome [7] is characterized by RBBB and abnormal ST waves in the anterior leads, including
- Arrhythmogenic right ventricular dysplasia [8] could also present with t-wave inversion in anterior leads. Arrhythmogenic right ventricular dysplasia (or cardiomyopathy) is characterized by fibro-fatty replacement of the right ventricular myocardium, and is associated with ventricular arrhythmias. EKG findings can include depolarization and/or repolarization changes in the right ventricular leads, including anterior t-wave inversion.
Take Home Points: Anterior t-wave inversion is common in children. In adult (females) it can be a normal variant. However, in the right clinical context, it also be associated with sudden death, PE, or myocardial ischemia, and therefore may merit further evaluation, particularly in patients with chest pain or suspicion for arrhythmia.
Submitted by Laura Wallace (@labellalaura), PGY-3
Edited by Maia Dorsett (@maiadorsett), PGY-3
Faculty Reviewed by Evan Schwarz
References:
1. Assali, A. R., Khamaysi, N., & Birnbaum, Y. (1997). Juvenile ECG pattern in adult black Arabs. Journal of electrocardiology, 30(2), 87-90.
2. Onat, T., Onat, A., & Can, G. (2008). Negative T wave in chest lead V1: relation to sex and future cardiovascular risk factors. Turk Kardiyol Dern Ars, 36(8), 513-518.
3. Hayden, G. E., Brady, W. J., Perron, A. D., Somers, M. P., & Mattu, A. (2002). Electrocardiographic T-wave inversion: differential diagnosis in the chest pain patient. The American journal of emergency medicine, 20(3), 252-262.
4. Aro, A. L., Anttonen, O., Tikkanen, J. T., Junttila, M. J., Kerola, T., Rissanen, H. A., ... & Huikuri, H. V. (2012). Prevalence and prognostic significance of T-wave inversions in right precordial leads of a 12-lead electrocardiogram in the middle-aged subjects. Circulation, 125(21), 2572-2577.
5. Migliore, F., Zorzi, A., Michieli, P., Marra, M. P., Siciliano, M., Rigato, I., ... & Corrado, D. (2012). Prevalence of cardiomyopathy in Italian asymptomatic children with electrocardiographic T-wave inversion at preparticipation screening. Circulation, 125(3), 529-538.
6. Mead, N. E., & O'Keefe, K. P. (2009). Wellen's syndrome: An ominous EKG pattern. Journal of Emergencies, Trauma and Shock, 2(3), 206.
7. Berne, P. (2012). Brugada syndrome. Circ J, 76(7), 1563-71.
8. Corrado, D., Buja, G., Basso, C., & Thiene, G. (2000). Clinical diagnosis and management strategies in arrhythmogenic right ventricular cardiomyopathy. Journal of electrocardiology, 33, 49-55.